2. Malnutrition
The ability to consume food is an essential and physiologically necessary human need. As it is commonly known, the quality of nutrition, its quantity and individual components will affect the condition of a body and have a preventive or modulating effect on selected diseases. A particular impact will also concern the ageing processes and physical capacity. Malnutrition is a disease leading to unfavourable changes, including body composition, physical and mental condition and also an element predicting a worse course of the underlying disease [
1].
There are many causes of malnutrition, but most often it is the result of accumulation of several of them. It affects 35-55% of hospitalized patients, and in the case of cancer even 40-90% of patients. Insufficient intake of nutrients, increased demand during illness or improper digestion and absorption processes are just some of the reasons, and their aetiology is much more complex [
2]. One of the key factors is inflammation associated with some disease [
6]. The nutritional status of patients was examined in the first week of hospital stay and then in the third week. The conclusions drawn indicate an increase in malnutrition from 46% to 76%, which also draws attention to the problem of hospital malnutrition [
7].
Elderly patients are a group particularly vulnerable to the development of malnutrition. Often they are people with multiple diseases, chronic inflammation, prolonged hospital stays and also changes occurring in the body on the level of hormones and enzymes. In addition to the above mentioned factors, there are also other factors such as economic conditions, which limit the possibility of consuming products and full-value meals or a difficult choice between nutrition and the purchase of medicines. All these occuring factors can additionally intensify poor physical well-being, but also mental state. Depression, low mood, suffering after the loss of relatives are problems that seniors struggle with on a daily basis, significantly affecting the deterioration of appetite and the general condition of the patient. Moreover, lack of teeth, problems with dentures or dysphagia create a physical barrier for them [
8]. It should also be mentioned that a large part of seniors spend the autumn years in care and treatment facilities or nursing homes, where up to 65% may be exposed to malnutrition. One of the main reasons may be insufficiently qualified and committed staff [
1]. Various causes of decreased appetite are suspected, not only a decrease in energy expenditure, but also an increased feeling of satiety [
9].
2.1. Types of Malnutrition
There are three types of malnutrition: kwashiorkor, marasmus and mixed.
a)
Kwashiorkor is characterized by abdominal swelling (so-called ascites) caused by disturbances in the acid-base and water-electrolyte balance. This may be related to the decreasing amount of proteins in the blood serum, mainly albumins. These molecules affect the oncotic pressure leading to water retention in the body. This also correlates with the increase in the ADH hormone and renin, which causes an increase in swelling [
10]. However, this is not the only cause of swelling, other factors are also necessary. Researchers point to the influence of the lymphatic system [
11]. Kwashiorkor most often develops rapidly, which is the result of increased catabolic changes. If it is left untreated, it may lead to death. Therapy consists of slowly correcting nutritional deficiencies, mainly electrolytes, microelements, protein, as well as preventing hypothermia and infections, and gradually expanding the diet [
10].
b)
Marasmus - otherwise known as protein-energy malnutrition. It develops slowly; it is manifested by a general decrease in food intake, which is often associated with the occurrence of infectious diseases (especially respiratory and gastrointestinal diseases). The first effect of the lack of nutrients is stunted growth (in children), followed by weight loss. This condition is characterized by loss of adipose tissue, reduced muscle mass as well as lack of edema and significant changes in visceral proteins. The concentration of albumin and plasma proteins is usually normal or slightly changed, despite a weight loss of 40% or more [
12].
c)
The mixed type is often diagnosed, especially in chronically ill patients [
13]. This type of malnutrition combines the clinical features of marasmus and kwashiorkor. It is characterized by the presence of oedema (with or without skin lesions), muscle atrophy and a decrease in subcutaneous fat tissue, as in the case of marasmus. During the nutritional process, the oedema subsides and the patients acquire clinical symptoms of marasmus [
12].
Cachexia, caused by a chronic disease (e.g. cancer), is also considered malnutrition. It is divided into following stages:
− during precachexia there is a loss of body weight less than or equal to 5% over a period of 6 months, chronic or temporary but recurrent inflammation (CRP> 5.0 mg/l) and symptoms such as loss of appetite and gastrointestinal problems, e.g. nausea or vomiting;
− a patient with cachexia has a weight loss of more than 5% or a BMI below 20 and a weight loss of more than 2% and 3 out of 5 other indicators such as fatigue, reduced muscle strength or mass, abnormal biochemical parameters or anorexia [
14].
The prognosis for survival is about three months. The triad of cachexia disorders is: continuous weight loss (it concerns in particular lean body mass), resistance to nutritional treatment and exacerbation of symptoms during a decline in condition. The pathogenesis of cancer cachexia is multifactorial. It concerns insufficient oral nutrition (often caused by anorexia), increased consumption, loss of micro- and macroelements by the body, improper functioning of metabolic processes, chronic inflammation and diametric changes caused by cancer treatment (radiotherapy or chemotherapy) [
15].
One of the effects of malnutrition may be sarcopenia, which is defined as a combination of unintentional decrease in muscle mass and skeletal muscle strength and function. It is usually diagnosed in geriatric patients. The most common causes of sarcopenia, apart from the patient's age, may be living conditions, inappropriate diet and pharmaceuticals. There are many terms that more precisely define the type of muscle-related disorders: amyotrophy, involution and dynapenia. One of the specific conditions is sarcopenic obesity, when despite the loss of muscle mass, there is an increase in adipose tissue. This condition may be difficult to diagnose due to an increase in body weight or its lack of change [
8].
Frailty syndrome should also be distinguished from malnutrition-related disorders. It is a mental and physical disorder that includes problems with mobility, chronic fatigue, unintentional weight loss, decreased physical activity as well as intellectual disability, usually observed in people over 60 years of age [
16].
2.2. Nutritional Status Assessment
Screening nutritional status allows for prevention of malnutrition, which will be an element as important as its treatment. The methods of assessing the patient's nutritional status are questionnaires - assessment scales, nutrition interview, as well as biochemical and anthropometric tests.
1) Nutritional questionnaires concern a.o. current body weight and its changes over six months, chronic diseases and the quantity and quality of food consumed. They are used to detect the presence of malnutrition and its severity [
3,
17].
a) Nutritional Scale Risk The Score (NRS 2002) includes data on weight loss over a specified period, current BMI and food intake, as well as correlations related to the severity of disease states. If the patient is over 70 years old, an additional point is added. The key to determining further intervention is the sum of points: if it is equal to or higher than 3, nutritional therapy should be implemented. If the sum is lower, the patient should be monitored and checked regularly. The maximum number of points is 7 [
3,
17].
b) The subjective global scale of nutritional assessment (SGA) consists of 3 points. Point 1 is an interview concerning age, height, body weight and gender, as well as changes in body weight, food intake, gastrointestinal symptoms, physical capacity and nutrient requirements resulting from the disease. Point 2 is a physical examination, and point 3 is a subjective summary of the patient's condition [
3].
Despite the statutory requirement to assess the nutritional status of patients based on the NRS 2002 or SGA scale, malnutrition is still too rarely detected or, despite detection, the necessary intervention is not implemented. Other questionnaires, not used as often as the above, are the MNA scale – Mini Nutritional Assessment and the MUST scale – Malnutrition Universal Screening Tool [
11]. A quick and easy to use tool is the SNAQ scale – Simplified Nutritional Appetite Questionnaire, which is based on the assessment of appetite and allows for the limitation of the expected weight loss [
17,
19].
2) Nutrition interview - properly conducted, allows for a more precise determination of the causes and errors made by the patient. It should include information on the quantity and regularity of meals, the amount of consumption of individual product groups (vegetables, fruit, dairy products, fish, meat, etc.), the amount of fluids consumed, gastrointestinal problems, the amount of sleep, physical activity, the method of processing and the quality of consumed products, as well as life and financial situation in order to objectively perceive and make real changes that can be introduced in the future. Important information that should not be omitted are previously used diets, comorbidities and medications taken [
3].
3) Anthropometric tests are a basic tool for monitoring physical parameters from the earliest years. Routine measurement of body mass and height accompanies a person from birth. BMI (body mass index) is the most commonly used. It is the quotient of body mass and height (squared). The results are interpreted in accordance with the developed standards (presented in
Table 1):
Malnutrition is defined at a value below 18.5. In elderly patients, a value below 23 will indicate the risk of malnutrition [
9].
Another method is to measure the skinfold above the triceps muscle. The presence of subcutaneous fat tissue with values lower than average (16.5-14.9 mm for women and 12.6-11.3 for men) indicates a decrease in the body's energy reserve. In turn, normal values for measuring the arm circumference are above 22 cm in women and 23 cm in men. A dynamometer is used to check how strong and efficient the patient's muscles are. Hand grip strength (HGS) is a standard parameter of hand function, which is assessed on a scale of 1-3. Together with other anthropometric indicators (such as body weight, height and BMI), it allows to complete the clinical picture of malnutrition [
18].
Bioimpedance allows for a full analysis of body composition. Through to the body composition test, it is possible to obtain precise data, in which the spectrum of error is much smaller. For example, when calculating BMI, body mass and height are used, and an athletic physique or suspected sarcopenic obesity are not assessed. In both cases, this measurement will indicate an unreliable result that may disturb further proceedings. Bioelectrical impedance is based on the difference in electrical resistance in adipose and non-fatty tissue (due to the presence of electrolytes and water), so thatthe following results are obtained: lean body mass, amount of adipose tissue, extra- and cellular masses, and water content. Depending on the type of device, there may be more parameters obtained, e.g. calculation of the basal metabolic rate or the amount of visceral adipose tissue. It is worth to mention patients, who have problems with movement, where carrying out the above measurements will be significantly difficult [
21].
For bedridden people, instead of height, the knee height measurement and bed scales are used, so that the staff does not have problems with transferring and the result is accurate. Calf circumference or WHR (the ratio of waist to hip circumference) is also often measured. There are many anthropometric methods – therefore, there will always be an appropriate one that can be individually adjusted to the patient and his needs. This undoubtedly requires well-trained medical personnel [
18].
4) Biochemical tests are one of the basic activities of diagnosing disorders of the body's functioning in the hospital. Due to their repeatability, they are also a good marker for detecting malnutrition, but also for monitoring the effects of its treatment.
a)
Albumin concentration in blood – is a commonly determined parameter among hospitalized patients. The normal range is 3.5 g/dl, and its decrease is an undesirable phenomenon that may indicate the risk of malnutrition. Despite various factors influencing their amount (medical condition and hydration level), a lower value is always treated as an unfavorable factor, especially in patients referred for surgery. Due to the half-life of 18 days and the connection with cytokine activity, it is rather an indicator of chronic malnutrition. Proteins with a shorter half-life are
transferrin and transthyretin (prealbumin). The latter is a protein transporting thyroid hormones, synthesized in the liver and partially catabolized by the kidneys. A serum prealbumin concentration below 10 mg/dl is associated with malnutrition. The main advantage of prealbumin compared to albumin is its shorter half-life (2-3 days), which makes it a more favorable marker of acute changes in nutritional status. Prealbumin levels may be elevated in cases of renal dysfunction, corticosteroid therapy, or dehydration, whereas they may be decreased during physiological stress, infection, liver dysfunction, and overhydration [
22,
23].
b)
Creatinine level reflects kidney function, but also muscle mass level. CHI = (urinary creatinine excretion/creatinine excretion estimated from height) × 100 shows muscle exhaustion (deficit) [
21,
22].
c)
Nitrogen balance is the difference between nitrogen taken in with food and excreted (through the kidneys and skin). The values obtained are interpreted as follows: negative balance – predominance of catabolism, positive balance – predominance of anabolism. This is influenced by the body's protein consumption, the presence of infection or kidney function, as well as the patient's physical condition (lying or moving) [
18,
21,
22].
d) As the disease intensifies and the patient's well-being worsens, the functioning of the immune system changes, as indicated by
the CLL, i.e.
total lymphocyte count. The normal value is more than 1500 in a cubic millimeter of peripheral blood, while values below 800 will be perceived as alarming [
18].
e)
Other parameters such as liver enzymes, lipid profile, electrolytes (calcium, potassium, sodium, chloride, phosphorus, magnesium), morphology and C-reactive protein level will allow for a broader look at the patient, also in the direction of anemia and other deficiencies [
21,
22].
2.3. Consequences of Malnutrition
As mentioned above, if malnutrition is treated improperly or left without intervention, will lead to death. This is often caused by irreversible changes that occur in the body during the entire process. Depending on the age of the patient, the effects will be different. Children diagnosed with malnutrition have a higher risk of mortality, reduced immunity to diseases caused by bacteria and viruses, but also mental skills [
24]. In adults, deficiencies of micro and macronutrients may contribute to the development of depression [
21].
Malnutrition in patients after severe injuries significantly increases catabolic changes. Cytokines and hormones such as epinephrine and cortisol are released, which among other things can increase energy expenditure by 50%. This also affects changes in protein metabolism and their conversion into energy, including muscle proteins. Consequently, if malnutrition has already occurred, it will continue to intensify. Due to the constant drawing of the body from protein stores, the ability of the body to renew cells decreases, wound healing is impaired, and changes in the immune system occur, such as the production of antibodies and the activity of white blood cells. Any loss of muscle will correlate with other effects; impairment of respiratory muscles causes a greater risk of pneumonia or respirator dependence [
7]. Reduction in heart muscle mass leads to reduced exercise capacity and circulatory failure. Insufficient supply of energy and nutrients will reduce the glomerular filtration rate and affect kidney function. The effects also affect the digestive system, due to the reduced absorption surface (lack of enterocyte stimulation by food), the absorption of mono- and disaccharides and fats is impaired , which leads to liver diseases [
21,
25].
Prevention of malnutrition should be the primary goal of medical personnel and the patient, because despite appropriate treatment, it will have its consequences. Education of doctors, nurses and other members of hospital teams and employment of dieticians allows for screening of patients at risk of malnutrition, but also for implementation of appropriate measures such as the entire process of nutritional treatment [
2].
3. Nutritional Treatment
Nutritional treatment precedes assessment of the patient's nutritional status, assessment of the demand for nutrients and determination of interventions, as well as creation of a nutritional plan consisting of the supply of appropriate amounts of macro- and micronutrients, ongoing monitoring and control of treatment results. The effect of a properly conducted scheme is the maintenance or improvement of the nutritional status in patients whose nutrition with a natural diet is insufficient, as well as, in some cases, treatment of the underlying disease [
3]. The possibility of implementing medical nutrition is based on one of the following conditions:
- expected inability to use an oral diet for more than 7 days;
- patient's malnutrition;
- expected inability to provide more than 60% of the recommended daily intake for a period exceeding 10 days [
3].
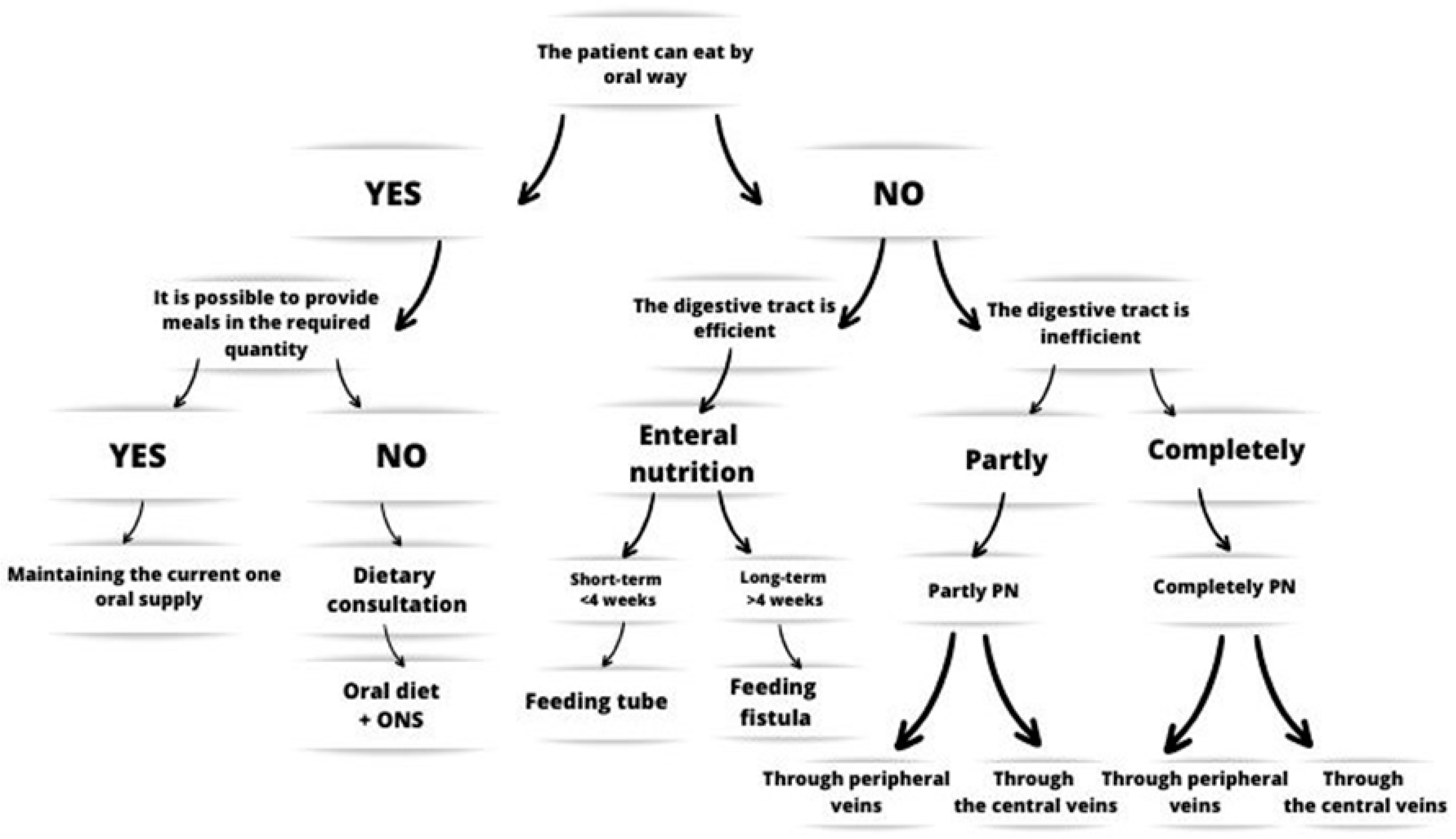
We distinguish oral, enteral and parenteral nutritional treatment, and with regard to the deployment in the patient, hospital and home nutrition. The nutritional treatment of the patient is based on the following algorithm:
Figure 1.
Algorithm of action in clinical nutrition, own development based on the Decision Scheme of Nutritional Treatment [
3].
Figure 1.
Algorithm of action in clinical nutrition, own development based on the Decision Scheme of Nutritional Treatment [
3].
3.1. Oral Nutritional Supplements
In the case where the patient does not consume adequate amounts of a natural diet, oral nutrition supplements are used. This is one of the types of a wide range of foods for special medical purposes. There are preparations that are complete in terms of ingredients or intentionally devoid of a selected component, e.g. fat. ONS are not intended to contain ingredients such as purines, lactose, gluten and cholesterol [
26]. When consuming ONS, the time of drinking them is an important factor (at least 30 minutes), it is also worth cooling them beforehand [
3].
Table 2.
Division of ONS, own study, based on literature [
26].
Table 2.
Division of ONS, own study, based on literature [
26].
| |
Preparation |
Characteristic |
| |
Hypocaloric |
about 0.5-0.9 kcal/ml |
| Classification according to caloric value. |
Isocaloric |
in the range of 0.9-1.2 kcal/ml |
| |
Hypercaloric |
about 1.3-2.4 kcal/ml |
| Classification depending on the amount of macronutrients |
High energy
High protein |
fat content increased by about 30%
protein content increased by at least 20% |
| |
Mixed |
- |
| |
Polymeric
|
polypeptides |
| Classification depending on the degree of protein hydrolysis. |
Oligomeric and monomeric |
oligopeptides and amino acids |
The wide range of products available on the market allows them to be selected for a specific disease entity. For patients with diabetes and glycemia disorders, there are products with a reduced content of monosaccharides, with a low glycemic index and containing added fiber. For people with liver diseases, low-fat or fat-free ONS can be intended, as well as with a modified fat profile and a reduced amount of protein, with the addition of BCAA (branched chain aminoacid), PUFA (polyunsaturated fatty acids), MUFA (monounsaturated fatty acids), MCT (medium chain triglycerides) and reduced aromatic amino acids. ONS for patients with kidney diseases are usually hypercaloric, low-protein and high-fat (mainly MCT), the amount of ingredients such as sodium, potassium, chlorine, calcium, phosphorus and magnesium, which could aggravate kidney problems, is reduced. In addition, there are supporting products, single-ingredient or incomplete, for example powdered fiber, which in many cases is difficult to provide to the diet naturally, as well as thickeners for the kitchen diet [
3]. Protein powder or glutamine is also available, which allows for enriching the natural diet.
Immunonutrition is characteristic for patients with neurological disorders. It is a regimen based on the supply of selected ingredients that have the ability to affect immunological and anti-inflammatory pathways [
27]. Preparations of this type contain: omega - 3 fatty acids, glutamine, arginine, nucleotides, antioxidants and prebiotic fiber. Omega-3 acids effectively reduce inflammation, influencing the overall improvement of treatment. Arginine takes part in protein synthesis, which is particularly important during the healing of wounds or pressure sores. The above-mentioned ingredients support the functioning of the immune system and the healing processes [
28].
It is worth mentioning the preparations that are intended for patients with difficult-to-heal wounds, ulcers, burns or pressure sores. They contain additives such as arginine, collagen and fatty acids that stimulate healing and regulate the immune system response. Ascorbic acid and microelements such as iron, zinc, as well as selenium or copper and individual vitamins also support wound healing [
29].
Depending on the companies offering the above preparations on the market, patients can choose ONS to suit their own preferences. This is a field of trade in a strong development phase, which allows for a wide range of effects and choices. Many products are available in liquid form, as well as individual powders to be mixed in selected solvents (milk, water, juices). Most ONS of one type have different flavors, from fruit to traditional ones such as caramel or chocolate [
30].
3.2. Enteral Nutrition
The concept of enteral nutrition includes the processes of oral nutrition (which was developed above), intragastric nutrition and enteral nutrition. Artificial nutrition through the digestive tract is used in malnourished patients who can not provide adequate oral intake. This type of nutrition requires the proper functioning of the digestive tract, the absence of obstruction, the possibility of using artificial access and the consent of the patient or the entity responsible for it [
30].
Indications include any disorders related to:
− dysphagia, the etiology of which may be different (neurodegenerative and neurological diseases, myasthenia, oncological diseases);
− diseases of the head and neck, as well as the upper digestive tract;
− the digestive tract or its partial obstruction, also with the processes of digestion and absorption (diseases of the pancreas, intestines, liver, allergies);
− chemotherapy and radiotherapy (cachexia or inflammatory reaction);
− chronic infections and diseases (COPD, organ failure);
- severe acute pancreatitis, loss of consciousness, extensive injuries and procedures [
30,
31,
32,
33].
The administration of an enteral diet requires its good tolerance.
Depending on the route and time of administration (over or under 14-21 days), the appropriate type of access to the gastrointestinal tract is selected for the patient's needs. In the case of patients who are expected to receive enteral nutrition for less than 2-3 weeks, a nasogastric or nasojejunal tube is inserted. Tubes can be made of various materials such as silicone or polyurethane. Sizes 8-12 F are used for nutrition, depending on the type of diet administered, equipped with guides. [
30,
34].
A nasogastric tube is used when there are no disorders of gastric emptying, and also if there is no reflux or neoplastic process. Due to its low price, simplicity of insertion and supply of preparations, it has a wide range of applications. Access will not be used in diseases and injuries in the craniofacial region and obstruction, and if the patient's hemodynamic stabilization is variable. Diets can be administered to the stomach by boluses (this is the most physiological supply) or by continuous infusion, preferably using pumps. A nasojejunal tube (intraduodenal or intestinal) is indicated in patients with reflux and gastroparesis , as well as with a risk of paralytic ileus or for use in the early period after surgery. This tube is more difficult to insert, and due to its smaller diameter, problems with its patency may occur more often. Preparations are administered to the intestine by continuous infusion. In patients who are expected to receive enteral nutrition for a longer period, permanent access to the stomach or intestine will be established. Gastrostomy can be inserted endoscopically, surgically or under ultrasound and X-ray control. PEG, or percutaneous endoscopic gastrostomy, is a minimally invasive procedure. It is used in patients with upper gastrointestinal tract injuries and is often inserted prophylactically when dysphagia or inflammatory reactions are anticipated. Jejunostomy is a shunt inserted into the small intestine, it can be used in cases of pyloric stenosis or after gastric resection. For each of the accesses inserted, when using the bolus or infusion method, it is necessary to remember about the night break. The effectiveness of selected actions should be assessed on an ongoing basis and any modifications should be introduced [
33,
34,
35].
Industrial diets are intended for artificial access. It is dangerous and medically unjustified to administer a natural kitchen diet, due to the increased risk of infection, access obstruction and lack of appropriate energy value, i.e. exposing the patient to deepening malnutrition [
36]. Depending on the patient's condition - the disease entity, the route and method of supply, as well as the efficiency of the gastrointestinal tract, an appropriate diet is selected. The composition of complete industrial preparations is based on similar ingredients:
- oligo- and polysaccharides derived mainly from starch, but also from beets, corn and cane;
- LCT (long chain triglycerides ), MCT, MUFA – vegetable oils;
- casein and whey proteins – in varying degrees of hydrolysis.
In patients requiring special interventions, preparations with modified amounts of macronutrients are selected [
37]. Industrial diets are divided depending on the degree of protein size into mono-, oligo- and polymeric, and into those assigned to a given disease entity (similarly to ONS). Standard diets are not hydrolyzed, which is why they are characterized by the lowest osmolarity. They are used in most patients, especially in the initial phase of nutrition. The content of macronutrients is similar to the proportions of the daily diet (15-20% of energy from proteins, 20-40% from fats, the rest from carbohydrates). In the case of modification of preparation components, the following diets are obtained: high-protein, high-energy and containing fiber, as well as with a specific fatty acid profile. Oligomeric preparations (containing short peptide chains) are characterized, apart from the hydrolyzed protein, also by a higher content of MCT acids, with an increased rate of digestion. Their osmolarity is 300-600 mOsmol /l. The last stage of protein hydrolysis, i.e. amino acids, contain monomeric diets, which is why their osmolarity is the highest [
34,
37]. Hemodialysis patients receive diets with increased calories, and the percentage of protein is also increased. In preparations for people with lung diseases, some carbohydrates are replaced with fats, which reduces carbon dioxide production and reduces the use of the mentioned organ. In oncological patients, as well as in perioperative care and transplantology, agents with added immunomodulating components are used [
37].
3.3. Parenteral Nutrition
In patients whose digestive tract can not be used or whose ability to use it is insufficient, parenteral nutrition is used [
38,
39]. The main indications for its introduction include intestinal failure or diseases related to them, which cause the inability to absorb an appropriate amount of the enteral diet, such as short bowel syndrome, Crohn's disease or radiation enteritis, surgical complications [
38].
Peripheral venous access is established in patients for no longer than 10-14 days or when the possibility of using central veins is excluded. Percutaneous catheters and vascular ports are used as central access. Mixtures administered to peripheral veins cannot exceed 900-1000 mOsm /l; all parenteral nutrition mixtures can be used in central veins [
38].
The parenteral nutrition planning scheme includes the time of feeding, the choice of venous access and the selection of a mixture appropriate to the patient's needs. The mixtures are based on amino acids, glucose, fat emulsion, and the necessary additives are water- and fat-soluble vitamins and trace elements. Immunomodulating substances such as omega-3 acids or glutamine may also be included. Depending on the type of bags, they differ in content and handling. Preparations prepared in the AIO and TIO (All in One; Two in One) mixer contain all the ingredients and are ready for administration. RTU (Ready To Use) bags should be prepared for connection in the hospital pharmacy in the laminar flow cabinet and the substances they do not contain (usually microelements and trace elements) should be injected into them [
38].
It is important to monitor blood glucose levels to avoid hypo- or hyperglycemia. Slow introduction of parenteral nutrition, frequent monitoring of blood glucose levels or the addition of insulin will help reduce excessive glucose levels. Hyperglycemia is expected in elderly patients with diabetes or multiple diseases. In the case of poorer tolerance or excessive lipid intake, hypertriglyceridemia is a common phenomenon. Risk factors include excess body weight, alcoholism, pancreatic diseases and taking certain medications. The permissible value is <400 mg/dl. As a preventive measure, it is recommended to add omega-3 fatty acids and reduce the supply of fats to a maximum of 1 g/kg bw /day [
38].
One of the most dangerous complications is the refeeding syndrome. It is characterized by disturbances in water and electrolyte balance, especially a decrease in phosphorus levels, often also thiamine, but also the occurrence of hypomagnesemia and hypokalemia. Risk factors include low BMI, weight loss, deficiencies, reduced energy intake for more than 5 days, as well as diseases that intensify catabolic changes in the body. Symptoms include edema, organ failure, and without an appropriate response, they lead to death. Prevention of RS includes the correction of electrolyte disturbances and deficiencies, slow introduction of nutrition starting with an energy value of 10-20 kcal/kg.bc, slowly increasing it to the target value, and continuous monitoring of the patient's condition [
38,
39,
40].
Parenteral nutrition-related liver impairment (PNALD) is encountered. The disease combinations may include cholestasis, steatosis and cholecystolithiasis. It may be manifested with abnormal liver parameters, steatosis, cirrhosis or, in the worst stage, fibrosis and liver failure. Lack of adequate supply of enteral diet affects the disturbance of bile flow and gallbladder function. Factors influencing increased risk include diseases and severe clinical condition of the patient, excessive supply of glucose and fats and excess omega-6 acids and phytosterols derived from soybean oil. The risk is reduced by the supply of omega-3 acids, as well as not overfeeding the patient and introducing enteral nutrition in the early phase [
30,
38].
Prevention of complications includes continuous monitoring of the patient's condition by checking the kidney and liver function, glycemia and electrolyte levels, at least once a week after a period of stabilization [
21,
38].
One of the diseases that affect high nutritional risk and increased catabolism in patients is acute pancreatitis. The older treatment regimen included the exclusion of oral nutrition in order to limit pancreatic secretion. Currently, according to ESPEN, properly conducted enteral nutrition can bring benefits such as improvement of clinical condition and shortening of hospital stay. Parenteral nutrition should be used when enteral diet is not tolerated or there are other contraindications to enteral nutrition. It is suspected that the use of ingredients such as glutamine and omega-3 acids may bring benefits [
21,
38]. A special group are surgical patients. Nutritional preparation for procedures lasting about 7-10 days is recommended. This improves the recovery period and faster mobilization of the gastrointestinal tract. Due to the variety of procedures in patients, perioperative nutrition will also change. In patients who are expected not to be able to provide more than 50% of the recommended daily intake by the enteral route, parenteral nutrition should be implemented. Each procedure carries a risk of postoperative complications, some of which will also be indications for the inclusion of PN, for example paralytic ileus and motility disorders. Additionally, according to ESPEN, PN supplementation with glutamine should be considered, which may shorten the hospital stay but does not affect mortality. In turn, the use of omega-3 acids reduces infections [
30,
38].
Due to the large number of chemical components, incorrectly selected doses or compounds may interact with each other and reduce the stability of the mixture and its quality, as well as pose a threat to the patient's life. The effects of chemical reactions between substrates may be:
− inactivation of vitamins;
− calcium precipitation;
- creaming of fat and separation of emulsion [
37]. In order to avoid the above effects, these drugs must be stored at a temperature of 2-8 degrees C and with limited exposure to light in order to limit oxidation [
38,
42].
4. Inflammation
Malnutrition, among others, increases the patient's risk of inflammation. The immune system is a protective barrier for the body against harmful factors such as bacteria or parasites. It includes mechanisms of specific response (innate and acquired immunity) and non-specific response (e.g. physical barriers such as skin, epithelium covering the digestive tract or respiratory tract, as well as secretions such as lysozyme or digestive enzymes). It includes lymphatic organs and glands [
43].
Inflammation can be called the body's response to injury, it is a defense mechanism to various factors (bacterial, physical and chemical) [
44]. Acute and chronic inflammation are distinguished, depending on the duration and active mechanism. Acute inflammation is characterized by a short period of time and the initiation of PMN cells (neutrophils), secretion of inflammatory mediators by mast cells (production of histamine, other vasoactive amines and proinflammatory cytokines) and macrophages (TNF-α, IL-1, PAF, nitric oxide, leukotrienes ), as well as components of the complement system (C3a, C4a, C5a). The effects include vascular changes such as vasodilation, which allows the free flow of plasma with antibacterial components and antibodies. Symptoms include fever, swelling, pain and hives. Once the cause of inflammation is excluded, repair processes are initiated, including the secretion of anti-inflammatory and pro-inflammatory cytokine inhibitors (IL-4, IL-10, TGF-β), as well as the secretion of collagen and growth factors by macrophages.
Innate immunity cells can rely on the pattern recognition receptor (PRR) system in various forms (soluble or present on the surface and in the cell). This is related to the mechanism of pathogen-associated molecular patterns (PAMPs) and tissue damage (DAMPs). Through binding of ligand to PRRs, signaling pathways are initiated that affect the activation of transcription factor (NF- kB) and interferon regulatory factors (IRFs), which leads to the initiation of the cellular response. This results in the secretion of pro-inflammatory cytokines, e.g. IL-1, IL-6, IL-10 or TNF-α and mediators (growth factors, interleukins, chemokines) [
4,
45].
Cytokines are diverse proteins secreted by immune system cells that affect the regulation of the inflammatory response in a specific way, as data transmitters or directly. They can also play homeostatic roles and participate in cell formation and maturation, and affect chemotaxis [
46]. Several types are distinguished depending on the producing cell: monokines, lymphokines, interleukins, chemokines , and interferons [
5].
Interferons, which protect against viruses by inhibiting replication - by limiting protein synthesis, are differentiated into two types I INF (INF-α and INF-β) and II INF (INF-γ). The antiviral activity of type I interferons was confirmed in studies. After infection of animals with the virus and administration of antibodies against interferon α and β, death occurred. They also affect the reduction of cell proliferation. INF-γ participates in the activation of the immune system, affects the differentiation of lymphocytes by acting on increased cytotoxicity, and also increases the phagocytic capacity of cells in another mechanism.
Lymphokines include IL-2 (growth factor necessary for the proliferation of T lymphocytes), IL-3 ( participation in hematopoiesis), IL-4 (growth factor necessary for the proliferation of B and Th2 lymphocytes), IL-5, IL-10, and IL-12.
Monokines are pro-inflammatory cytokines such as IL-1, IL-6, IL-8, IL-12 TNF-α. Their main tasks are to influence:
- increased body temperature,
-increased phagocytosis,
- secretion of acute phase proteins (CRP and MBP),
- opsonization action and complement system action.
Chemokines play a special role in the chemotaxis of selected cells of the immune system such as lymphocytes, neutrophils and monocytes.
An important element is maintaining balance in the functioning of the immune system. Too high levels of secreted cytokines have been observed in mental disorders . This can affect tissue damage, contributing to neurodegenerative and autoimmune diseases [
5]. The influence of immunity on cancer cells is also discussed, one of the factors of their development is chronic inflammation. Individual cytokines can act in a given way, for example IL-1α and IL-1β are involved in the secretion of carcinogenic substances such as reactive oxygen species or nitric oxide [
47]. A disease affecting a large part of society is inflammatory bowel disease, factors influencing the occurrence of the disease include smoking, inappropriate diet or genetic factors, their accumulation leads to dysfunction of the intestinal barrier, which affects the movement of microorganisms and the initiation of immune cell activity. Characteristic cytokines for this process are TNF-α, IL-6 and IL-23 [
48]. The action of IL-6 can be pro- or anti-inflammatory (depending on the secreted dose), it is used as a marker of inflammation in oncological patients and those burdened with autoimmune diseases, due to its key role in the activation of the immune system [
49]. It is an unfavorable prognostic factor in diseases of the circulatory system and pancreas [
4]. It reduces the production of proteins such as albumin, transferrin and fibronectin and regulates the level of zinc and iron in serum [
50]. It affects liver regeneration and its proper functioning, but its chronic activation can lead to the development of cancer cells [
61]. TNF-α affects the secretion of acute phase proteins, especially in burns, and also has a prothrombotic effect [
4,
52].
Inflammation adversely affects the patient's nutritional status. It has been shown that nutritional therapy with CRP > 100 mg/dl did not have a beneficial effect on mortality within 30 days. This highlights the need for simultaneous action on treating the underlying disease, calming the inflammation, but also taking care to stop the loss of muscle mass and continuously compensate for deficiencies [
6].
4. Immunomodulating Ingredients
Many immunomodulating ingredients have an impact on improving the functioning of the immune system, this may include reducing inflammation, increasing resistance to infectious agents, and increasing MALT (mucosa associated lymphoid tissue ) activity and counteracting SIRS (systemic inflammatory reaction syndrome ). In the long term, this will shorten the hospital stay and improve the nutritional status [
53,
54,
55].
Arginine is synthesized in the liver, kidneys, and enterocytes. It is also supplied exogenously. It participates in the synthesis of nucleotides and stimulates the activity of lymphocytes and hormones. In cachectic patients, its deficiency occurs [
56,
57]. This amino acid also participates in the production of nitric oxide and citrulline and in the ornithine cycle [
53]. It may have a beneficial effect on therapies in many diseases, including diabetes or wound healing [
57]. The dose that improves the functioning of the immune system is 3-4 times higher than the intake from conventional food, which is about 5.5 g [
28].
In the case of increased catabolism, the production of endogenous glutamine may be impaired and insufficient. It is a basic energy for the differentiation of intestinal epithelial cells and a source of energy for lymphocytes and macrophages, therefore, deficiency may result in ulceration of structures, intestinal villus atrophy and intestinal barrier leakage. Exogenous supply of glutamine reduces protein breakdown and improves the process of their synthesis. Connecting of the above processes improves immunity and reduces the occurrence of infections [
58,
59,
60]. Glutamine has a beneficial effect on parameters such as mortality, infections and the length of hospital stay in surgical patients [
28].
Omega-3 acids, i.e. eicosapentaenoic acid, docosahexaenoic acid and alpha-linolenic acid, are exogenous compounds. They are building components of cell membranes and participate in transport processes at the cellular level, supporting the functioning of the nervous system [
61]. By occuring in the cell, they may reduce the pro-inflammatory effect of some factors and improve its functioning. They are characterized by antithrombotic, anti-allergic effects and have a beneficial effect on the lipid profile - they significantly reduce the level of triglycerides [
62]. Prostaglandins E and leukotrienes B
4 are created from omega-6 acids, which affect the inflammation. In turn, a higher supply of omega-3 acids reduces the risk of chronic inflammatory diseases and reduces the amount of secreted pro-inflammatory cytokines [
28,
62,
63]. A characteristic effect is also observed in cancer diseases. In oncology patients, abnormal levels of omega-6 acids have been detected, which in the presence of cyclooxygenase 2 transform into eicosanoids that affect the growth of tumors. Omega-3 acids reduce the production of prostaglandin E2, which leads to the spread of cancer [
63]. They can also improve the effectiveness of radiotherapy and chemotherapy [
64]. However, there is no hard evidence of a reduction in the incidence of cancer despite supplementation with omega-3 acids [
65]. It has been shown that DHA is more effective in improving the lipid profile and selected inflammatory markers than EPA [
61]. It may also have a beneficial effect on weight loss. The addition of EPA and DHA supplementation combined with appropriate exercise and a healthy diet significantly reduced the percentage of adipose tissue and abdominal skin folds in the study group compared to the control group [
66].
Vitamin D is one of the fat-soluble vitamins. It has a multifaceted effect, its deficiency is associated with an increased risk or exacerbation of autoimmune diseases, cardiovascular system and skeletal system. It can affect the secretion (IL-4, IL-5, IL-10) and inhibit the secretion (IL-12, IL-6, TNF-α) of selected cytokines. A proper level of vitamin D in the serum reduces the incidence of influenza and the severity of COVID-19 [
67,
68,
69], similar correlations are also sought in the treatment of neoplastic diseases, such as reducing the occurrence of micrometastases [
68].
Vitamin E has a regulating effect on the immune system by strengthening the cellular and humoral response, reducing the secretion of proinflammatory cytokines (IL-6, TNF-α) and changing the integrity of mucous membranes, thanks to which the function of transmitting external signals to the cell functions properly. The role of vitamin E in reducing the risk of respiratory infections, as well as some allergic diseases such as asthma, has been suggested [
70,
71].
Nucleotides, which participate in many biochemical processes, are components of coenzymes, triphosphates and are the building material of nucleic acids DNA and RNA. Their influence includes beneficial effects on the gastrointestinal tract, such as the functioning of the GALT system, regeneration of intestinal villi and mucosa, as well as limiting bacterial translocation [
53]. Nucleotide supply may also affect the maturation of T lymphocytes and the expression of IL-2, IL-6, IL-8 [
21,
28]. A diet enriched with nucleotides correlates with a reduced frequency of complications and a shorter hospital stay, especially in cancer patients undergoing surgical procedures [
21].
Vitamin C shortens the duration of infection and reduces the severity of symptoms, protects cells from excessive oxidation, and supports the function of lymphocytes and phagocytes [
72]. It also has antithrombotic and antiviral effects, and has been suggested to have a beneficial effect on the host response to the SARS-CoV-2 virus [
73]. Ascorbic acid stabilizes the collagen structure, which may be beneficial in the healing process of wounds and pressure sores [
29].
The role of magnesium is known in many body processes such as DNA and RNA replication, enzyme activation, cell membrane stabilization, and muscle contraction. Magnesium also affects immune processes such as reduced cytokine secretion by monocytes, proliferation, and lymphocyte development. In turn, magnesium deficiency has been observed to increase the level of proinflammatory cytokines such as IL-6, TNF-α, IL-β, CRP and reduce antioxidant potential, increasing exposure to free radicals [
74,
75,
76]. It is suspected that magnesium deficiency may affect the occurrence of diseases such as insulin resistance, type II diabetes, and cardiometabolic syndrome [
76].
Selenium may have a preventive effect on cancer and neurodegenerative diseases, it is involved in processes related to the functioning of the thyroid gland and the immune system. Selenium deficiency reduces the effectiveness of the immune response to infections and reduces the activity of selected cells such as T lymphocytes, macrophages and NK cells [
74]. Selenium is particularly believed to have a beneficial effect on autoimmune thyroiditis, it affects the reduction of the level of antibodies against thyroid peroxidase [
77].
Zinc is a coenzyme and a component regulating the activity of enzymes, it participates in the synthesis of proteins, DNA and RNA. The immunological activity of zinc has a multifaceted effect, among others it supports the activity of NK cells (their correct number and activity of chemotaxis and lysis of unwanted cells), and also participates in the maturation of T lymphocytes. In the case of chronic inflammation in systemic diseases, zinc deficiency may increase the secretion of cytokines IL-β, IL-1α and IL-6 (zinc supplementation may reduce its level in serum [
78]) [
74], and also affects the impairment of cellular and humoral response, reducing resistance to infections [
79].