Submitted:
13 December 2024
Posted:
14 December 2024
Read the latest preprint version here
Abstract
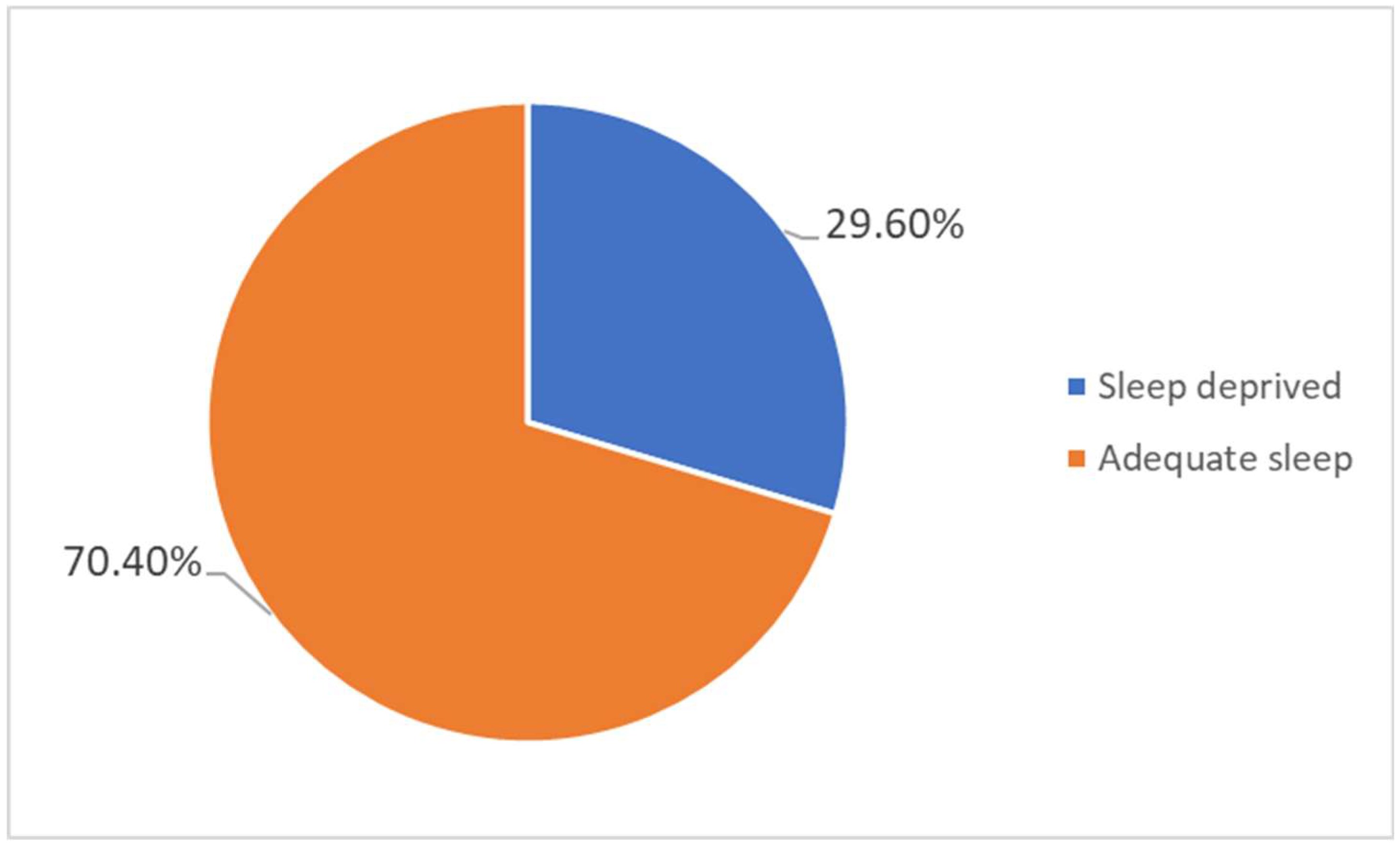
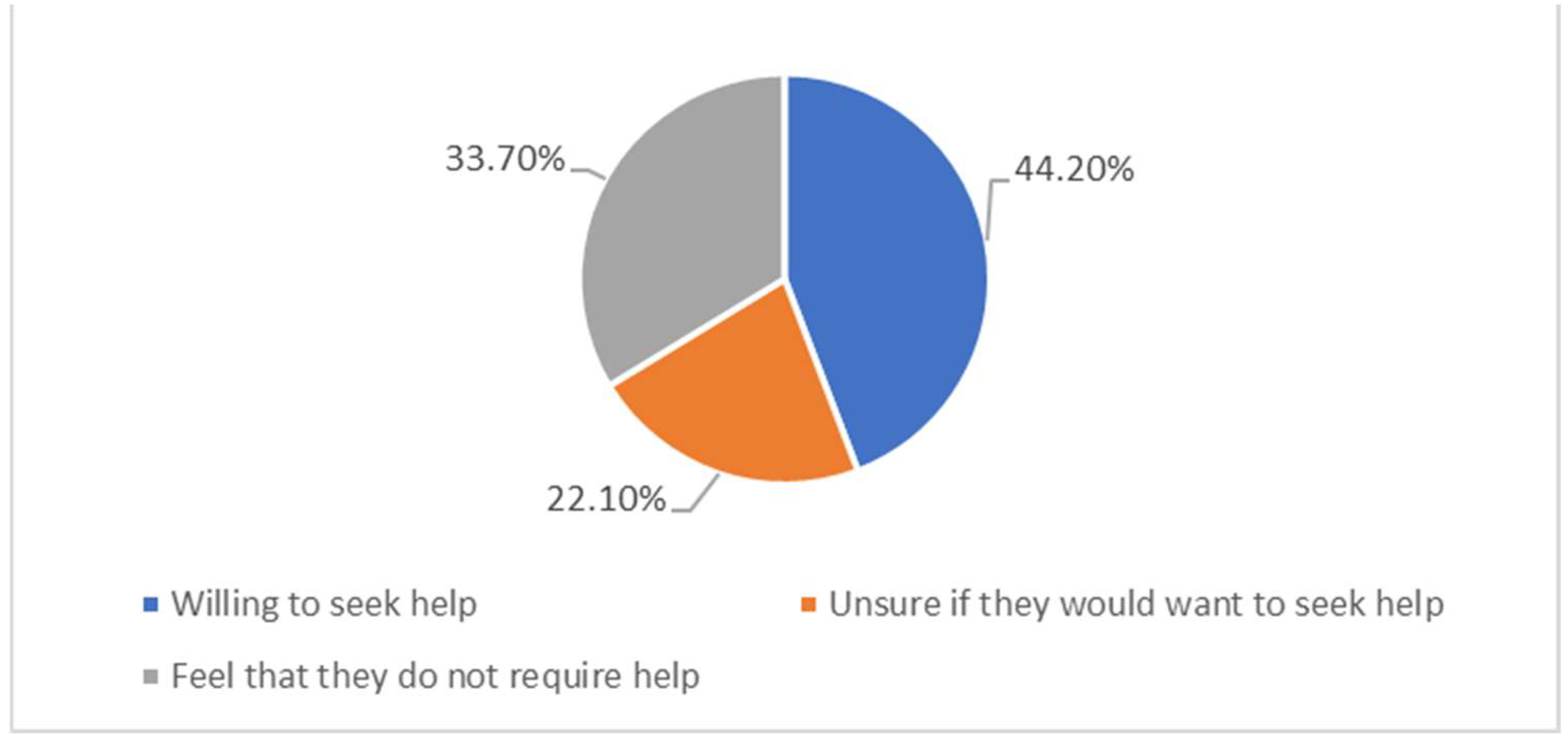
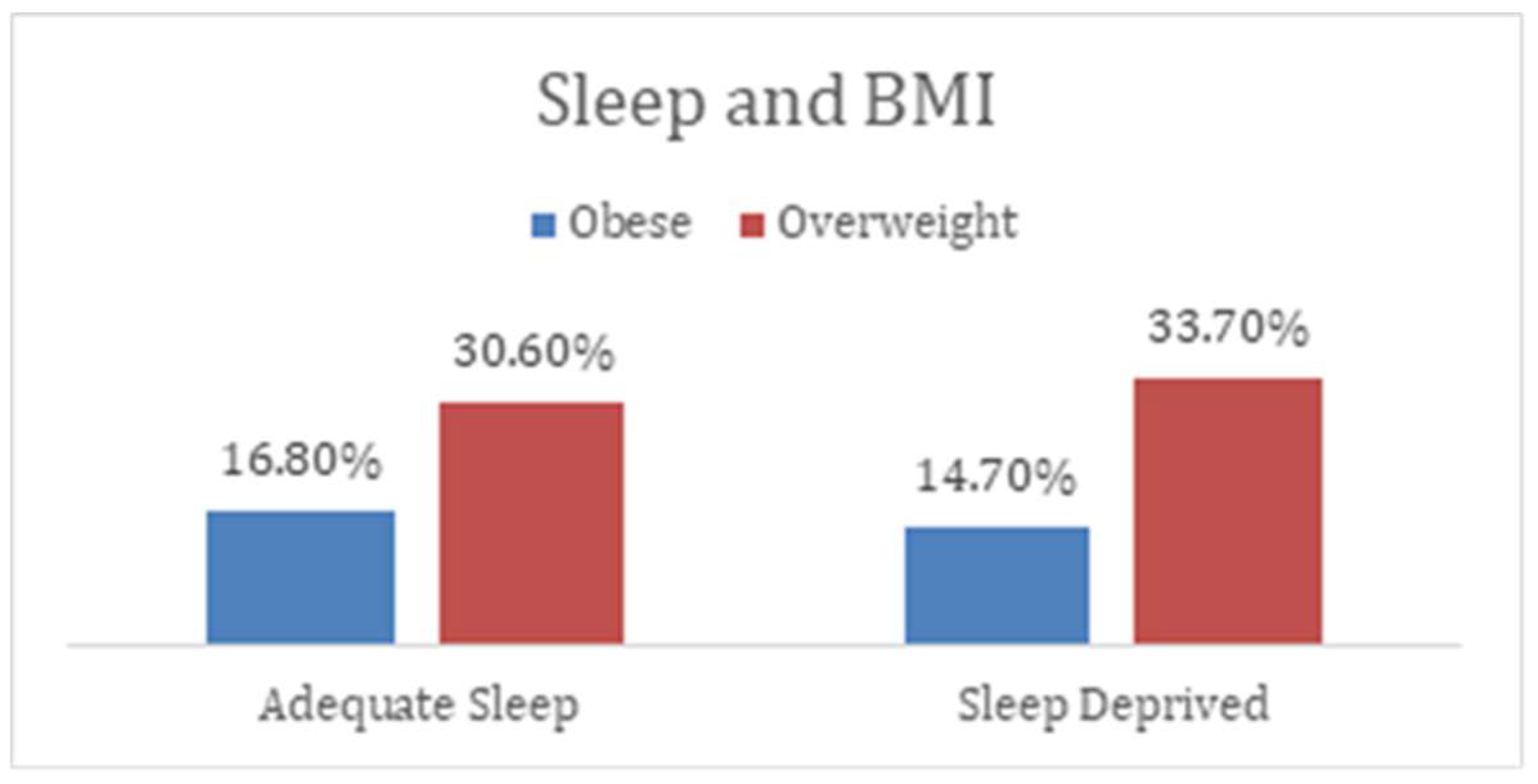
Background: Sleep deprivation is a global health concern with clinical, economic, and social consequences. Studies conducted in Asia reported a significant prevalence of poor sleep quality. There is a paucity of data on sleep deprivation in the Middle East and UAE, in particular. We set out to determine the prevalence of sleep deprivation and its association with physical and mental health in UAE. Methods: We used a cross-sectional design with a sample size, estimated using StatCalc software. Data collection tool was a survey instrument that we developed and then validated. Data analysis was done using Statistical Package for Social Sciences (SPSS). Results: Nearly 51% of the participants were younger than 25 years. Sleep deprived participants reported experiencing headaches frequently (25%) with a p-value of 0.07, with 22% having feelings of depression and lack of concentration with a p-value of 0.016. Discussion: sleep deprivation showed an association with depression/hopelessness but not statistically significant. However, sleep-deprived individuals may be more prone to physical and mental health conditions in the long term, requiring further research. Conclusion: This study establishes a link between sleep deprivation and physical/mental health outcomes, requiring further research. The willingness of many sleep-deprived individuals to seek help offers a promising avenue for intervention. Policymakers ought to integrate sleep health into broader public health policy.
Keywords:
1. Introduction
- -
- To determine the effect of sleep deprivation on mental health among adults in the UAE.
- -
- To determine the effect of sleep deprivation on physical health among adults in the UAE.
- -
- To determine the primary contributing factors that cause sleep deprivation
- -
- To investigate modifiable behaviour patterns that can improve sleep deprivation
- -
- To generate evidence to aid policy and public health education
2. Materials and Methods:
2.1. Study Design
2.2. Research Methods
2.3. Population and Sample
2.4. Data Collection and Tool
2.5. Ethics Approval
2.6. Data Analysis
3. Results:
3.1. Demographics
3.2. Sleep Deprivation and Physical Health
3.3. Sleep Deprivation and Mental Health
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- CDC. (2024, ). About Sleep. Sleep. https://www.cdc.gov/sleep/about/?CDC_AAref_Val=https://www.cdc.gov/sleep/about_sleep/how_much_sleep. 2 April.
- More than 40% of UAE residents are not getting enough quality sleep. (2024). Premierinn.com. https://mena.premierinn.
- Badri, M.; Al Khaili, M.; Aldhaheri, H.; Yang, G.; Albahar, M.; Alrashdi, A. From good sleep to health and to quality of life– path analysis of determinants of sleep quality of working adults in Abu Dhabi. Sleep Science and Practice 2023, 7. [Google Scholar] [CrossRef]
- Nasim, M.; Saade, M.; AlBuhairan, F. Sleep deprivation: prevalence and associated factors among adolescents in Saudi Arabia. Sleep Medicine 2019, 53, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Keyes, K.M.; Maslowsky, J.; Hamilton, A.; Schulenberg, J. The Great Sleep Recession: Changes in Sleep Duration Among US Adolescents, 1991-2012. PEDIATRICS 2015, 135, 460–468. [Google Scholar] [CrossRef]
- Rey-López, J.P.; de Carvalho, H.B.; de Moraes AC, F.; Ruiz, J.R.; Sjöström, M.; Marcos, A.; Polito, A.; Gottrand, F.; Manios, Y.; Kafatos, A.; Molnar, D.; Widhalm, K.; De Henauw, S.; Moreno, L.A. Sleep time and cardiovascular risk factors in adolescents: The HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study. Sleep Medicine 2014, 15, 104–110. [Google Scholar] [CrossRef]
- Chen, T.; Wu, Z.; Shen, Z.; Zhang, J.; Shen, X.; Li, S. Sleep duration in Chinese adolescents: biological, environmental, and behavioural predictors. Sleep Medicine 2014, 15, 1345–1353. [Google Scholar] [CrossRef]
- Ohida, T.; Osaki, Y.; Doi, Y.; Tanihata, T.; Minowa, M.; Suzuki, K.; Wada, K.; Suzuki, K.; Kaneita, Y. An Epidemiologic Study of Self-Reported Sleep Problems among Japanese Adolescents. Sleep 2004, 27, 978–985. [Google Scholar] [CrossRef]
- Al-Haifi, A.A.; Al-Majed, H.T.; Al-Hazzaa, H.M.; Musaiger, A.O.; Arab, M.A.; Hasan, R.A. Relative Contribution of Obesity, Sedentary Behaviours and Dietary Habits to Sleep Duration Among Kuwaiti Adolescents. Global Journal of Health Science 2015, 8, 107. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazzaa, H.M.; Musaiger, A.O.; Abahussain, N.A.; Al-Sobayel, H.I.; Qahwaji, D.M. Lifestyle correlates of self-reported sleep duration among Saudi adolescents: a multicentre school-based cross-sectional study. Child: Care, Health and Development 2013, 40, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Al-Jahdali, F.; AlALwan, A.; Abuabat, F.; Bin Salih, S.; Al-Harbi, A.; Baharoon, S.; Khan, M.; Ali, Y.; Al-Jahdali, H. Prevalence of sleep duration among Saudi adults. Saudi Medical Journal 2017, 38, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.Y.; Lau, J.H.; Vaingankar, J.A.; Sambasivam, R.; Shafie, S.; Chua, B.Y.; Chow, W.L.; Abdin, E.; Subramaniam, M. Sleep quality of Singapore residents: Findings from the 2016 Singapore mental health study. Sleep Medicine: X 2022, 4, 100043. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.C.; Hsu, N.W.; Chou, P. Subgrouping Poor Sleep Quality in Community-Dwelling Older Adults with Latent Class Analysis - The Yilan Study, Taiwan. 5432; 10. [Google Scholar] [CrossRef]
- Doi, Y. , Minowa, M. , Uchiyama, M., & Okawa, M. (2001). Subjective sleep quality and sleep problems in the general Japanese adult population. Psychiatry and Clinical Neurosciences 2020, 55, 213–215. [Google Scholar] [CrossRef]
- Liao, Y.; Xie, L.; Chen, X.; Kelly, B.C.; Qi, C.; Pan, C.; Yang, M.; Hao, W.; Liu, T.; Tang, J. Sleep quality in cigarette smokers and nonsmokers: findings from the general population in central China. BMC Public Health 2019, 19. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Liao, Y.; Kelly, B.C.; Xie, L.; Xiang, Y.-T.; Qi, C.; Pan, C.; Hao, W.; Liu, T.; Zhang, F.; Chen, X. Gender and Regional Differences in Sleep Quality and Insomnia: A General Population-based Study in Hunan Province of China. Scientific Reports 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- WONG; WS; FIELDING; R Prevalence of insomnia among Chinese adults in Hong Kong: a population-based study. Journal of Sleep Research 2011, 20(1pt1), 117–126. [CrossRef]
- Self-reported sleep quality in a multi-ethnic Asian population. (2017). Journal of Sleep Research, 26, 14–14. [CrossRef]
- In recognition of World Sleep Day, Philips presents its annual global sleep survey results. (n.d.). Philips. https://www.philips.com/a-w/about/news/archive/standard/news/press/2019/20190307-in-recognition-of-world-sleep-day-philips-presents-its-annual-global-sleep-survey-results.
- World Health Organization. (2024). Constitution of the world health organization. World Health Organization. https://www.who.
- World Health Organization: WHO. (2010, ). A healthy lifestyle - WHO recommendations. https://www.who. 6 May.
- Cooper, C.B.; Neufeld, E.V.; Dolezal, B.A.; Martin, J.L. Sleep deprivation and obesity in adults: a brief narrative review. BMJ Open Sport & Exercise Medicine 2018, 4, e000392. [Google Scholar] [CrossRef]
- Chaput, J.; Dutil, C.; Featherstone, R.; Ross, R.; Giangregorio, L.; Saunders, T.J.; Janssen, I.; Poitras, V.J.; Kho, M.E.; Ross-White, A.; Carrier, J. Sleep duration and health in adults: an overview of systematic reviews. Applied Physiology Nutrition and Metabolism 2020, 10 (Suppl. 2)), S218–S231. [Google Scholar] [CrossRef]
- Kripke, D.F. Short and long sleep and sleeping pills. Archives of General Psychiatry 1979, 36, 103. [Google Scholar] [CrossRef] [PubMed]
- Medic, G. , Wille, M., & Hemels, M. E. (2017, ). Short- and long-term health consequences of sleep disruption. Nature and science of sleep. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5449130/#:~:text=have%20been%20reported. 19 May.
- Balushi, M. A. , Balushi, S. A., Javaid, S.,et.al. Association between depression, happiness, and sleep duration: data from the UAE healthy future pilot study. BMC Psychology 2022, 10. [CrossRef]
- Vats, M.G.; Mahboub, B.H.; Hariri, H.A.; Zaabi, A.A. ; Vats D (2016) Obesity Sleep-Related Breathing Disorders in Middle East, U.A.E. Canadian Respiratory Journal, 2016, 1–5. [CrossRef]
- Good health and well-being | The Official Portal of the UAE Government. (n.d.). https://u.ae/en/about-the-uae/leaving-no-one-behind/3goodhealthandwellbeing.
- Introduction | StatCalc | User Guide | Support | EPI InfoTM | CDC. (n.d.). https://www.cdc.gov/epiinfo/user-guide/statcalc/statcalcintro.html.
- Stanford Medicine (2024), Pfizer Inc. - PHQ-9 Patient Depression Questionnaire, https://med.stanford.edu/fastlab/research/imapp/msrs/_jcr_content/main/accordion/accordion_content3/download_256324296/file.res/PHQ9%20id%20date%2008.03.
- Buchanan, B. (2024b, September 9). Generalised Anxiety Disorder Assessment (GAD-7). NovoPsych. https://novopsych.com.au/assessments/anxiety/generalised-anxiety-disorder-assessment-gad-7.
- https://www.pfizer.com/news/press-release/press-release-detail/pfizer_to_offer_free_public_access_to_mental_health_assessment_tools_to_improve_diagnosis_and_patient_care.
- IBM SPSS Statistics. (n.d.). https://www.ibm.com/products/spss-statistics?utm_content=SRCWW&p1=Search&p4=43700077616110376&p5=e&p9=58700008513382664&gad_source=1&gclid=Cj0KCQjwpvK4BhDUARIsADHt9sRhNHK_UfgTZl79Rd-tjasfH0edAro57R9YrUo5cpYI9QMzSamDy8QaArfqEALw_wcB&gclsrc=aw.
- https://www.researchgate.net/figure/Age-group-comparison-between-Young-adult-18-25-age-Adult-26-44-age-Middle-age_tbl1_338842581.
- Roberts, R.E.; Duong, H.T. The Prospective Association between Sleep Deprivation and Depression among Adolescents. SLEEP 2014, 37, 239–244. [Google Scholar] [CrossRef]
- World Health Organization: WHO. (2010, May 6) A healthy lifestyle - WHO recommendations. https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations.
- WONG; WS; FIELDING; R Prevalence of insomnia among Chinese adults in Hong Kong: a population-based study. Journal of Sleep Research 2011, 20(1pt1), 117–126. [CrossRef]
- Hanson, J. A., & Huecker, M. R. (2023, June 12). Sleep deprivation. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK547676/.
- Xiao, Q. , Arem, H., Moore, S. C., Hollenbeck, A. R., & Matthews, C. E. (2013c). A large prospective investigation of sleep duration, weight change, and obesity in the NIH-AARP Diet and Health Study cohort. American Journal of Epidemiology, 1610. [Google Scholar] [CrossRef]
- Wu, Y.; Zhai, L.; Zhang, D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Medicine 2014, 15, 1456–1462. [Google Scholar] [CrossRef]
- Gangwisch, J.E.; Malaspina, D.; Boden-Albala, B.; Heymsfield, S.B. Inadequate sleep as a risk factor for obesity: Analyses of the NHANES i. SLEEP 2005, 28, 1289–1296. [Google Scholar] [CrossRef]
- Chattu, V.; Manzar, M.; Kumary, S.; Burman, D.; Spence, D.; Pandi-Perumal, S. The global problem of insufficient sleep and its serious public health implications. Healthcare 2018, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Geiger, S.D.; Sabanayagam, C.; Shankar, A. The Relationship between Insufficient Sleep and Self-Rated Health in a Nationally Representative Sample. Journal of Environmental and Public Health 2012, 2012, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Engeda, J.; Mezuk, B.; Ratliff, S.; Ning, Y. Association between duration and quality of sleep and the risk of pre-diabetes: evidence from NHANES. Diabetic Medicine 2013, 30, 676–680. [Google Scholar] [CrossRef] [PubMed]
- Yoda, K.; Inaba, M.; Hamamoto, K.; Yoda, M.; Tsuda, A.; Mori, K.; Imanishi, Y.; Emoto, M.; Yamada, S. Association between Poor Glycemic Control, Impaired Sleep Quality, and Increased Arterial Thickening in Type 2 Diabetic Patients. PLoS ONE 2015, 10, e0122521. [Google Scholar] [CrossRef]
- Iyegha, I. D. , Chieh, A. Y., Bryant, B. M., & Li, L. (2019b). Associations between poor sleep and glucose intolerance in prediabetes. Psychoneuroendocrinology 2019, 110, 104444. [Google Scholar] [CrossRef] [PubMed]
- Humans.Txt. (n.d.). Oman Medical Journal-Archive. https://omjournal.org/articleDetails.aspx?coType=1&aId=1825.
- Spiegel, K.; Leproult, R.; Van Cauter, E. Impact of sleep debt on metabolic and endocrine function. The Lancet 1999, 354, 1435–1439. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, D., & Pacheco, D. (2023, October 26). Lack of sleep and diabetes. Sleep Foundation. https://www.sleepfoundation.org/physical-health/lack-of-sleep-and-diabetes.
- Dutil, C.; Chaput, J. Inadequate sleep as a contributor to type 2 diabetes in children and adolescents. Nutrition and Diabetes 2017, 7, e266. [Google Scholar] [CrossRef] [PubMed]
- Moon, C.; Hagen, E.W.; Johnson, H.M.; Brown, R.L.; Peppard, P.E. Longitudinal sleep characteristics and hypertension status: results from the Wisconsin Sleep Cohort Study. Journal of Hypertension 2020, 39, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Gangwisch, J.E.; Heymsfield, S.B.; Boden-Albala, B.; Buijs, R.M.; Kreier, F.; Pickering, T.G.; Rundle, A.G.; Zammit, G.K.; Malaspina, D. Short sleep duration as a risk factor for hypertension. Hypertension 2006, 47, 833–839. [Google Scholar] [CrossRef]
- Covassin, N.; Singh, P. Sleep duration and cardiovascular disease risk. Sleep Medicine Clinics 2016, 11, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Covassin, N.; Singh, P. Sleep duration and cardiovascular disease risk. Sleep Medicine Clinics 2016, 11, 81–89. [Google Scholar] [CrossRef]
- Hsu, M.; Lee, K.; Lin, T.; Liu, W.; Ho, S. Subjective sleep quality and association with depression syndrome, chronic diseases and health-related physical fitness in the middle-aged and elderly. BMC Public Health 2021, 21. [Google Scholar] [CrossRef] [PubMed]
- Poor sleep quality increases inflammation, community study finds. (2010, November 10). ScienceDaily. https://www.sciencedaily.com/releases/2010/11/101114161939.htm.
- Dzierzewski, J.M.; Donovan, E.K.; Kay, D.B.; Sannes, T.S.; Bradbrook, K.E. Sleep inconsistency and markers of inflammation. Frontiers in Neurology 2020, 11. [Google Scholar] [CrossRef]
- Song, T.; Yun, C.; Cho, S.; Kim, W.; Yang, K.I.; Chu, M.K. Short sleep duration and poor sleep quality among migraineurs: A population-based study. Cephalalgia 2017, 38, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Kelman, L.; Rains, J.C. Headache and Sleep: Examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache the Journal of Head and Face Pain 2005, 45, 904–910. [Google Scholar] [CrossRef] [PubMed]
- Whale, K.; Gooberman-Hill, R. The importance of sleep for people with chronic pain: Current insights and evidence. JBMR Plus 2022, 6. [Google Scholar] [CrossRef]
- Edwards, R.R.; Almeida, D.M.; Klick, B.; Haythornthwaite, J.A.; Smith, M.T. Duration of sleep contributes to next-day pain report in the general population ☆. Pain 2008, 137, 202–207. [Google Scholar] [CrossRef]
- Vinstrup, J.; Jakobsen, M.D.; Calatayud, J.; Jay, K.; Andersen, L.L. Association of stress and musculoskeletal pain with poor sleep: Cross-Sectional study among 3,600 hospital workers. Frontiers in Neurology 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Vinstrup, J.; Jakobsen, M.D.; Andersen, L.L. Poor Sleep Is a Risk Factor for Low-Back Pain among Healthcare Workers: Prospective Cohort Study. International Journal of Environmental Research and Public Health 2020, 17, 996. [Google Scholar] [CrossRef] [PubMed]
- Haack, M.; Simpson, N.; Sethna, N.; Kaur, S.; Mullington, J. Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology 2019, 45, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Marks, H. (2022, August 2). Sleep deprivation and memory loss. WebMD. https://www.webmd.com/sleep-disorders/sleep-deprivation-effects-on-memory.
- Alhola, P. , & Polo-Kantola, P. (2007, October 1). Sleep deprivation: Impact on cognitive performance, 1 October 2656. [Google Scholar]
- Chen, P.; Ban, W.; Wang, W.; You, Y.; Yang, Z. The Devastating Effects of Sleep Deprivation on Memory: Lessons from Rodent Models. Clocks & Sleep 2023, 5, 276–294. [Google Scholar] [CrossRef] [PubMed]
- Tomaso, C.C.; Johnson, A.B.; Nelson, T.D. The effect of sleep deprivation and restriction on mood, emotion, and emotion regulation: three meta-analyses in one. Sleep. 2021 Jun 11;44:zsaa289. [CrossRef] [PubMed] [PubMed Central]
- Killgore, W.D.; Balkin, T.J.; Wesensten, N.J. Impaired decision making following 49 h of sleep deprivation. J Sleep Res. 2006 Mar;15:7-13. [CrossRef] [PubMed]
- Taghvaee, L.; Mazandarani, A.A. Poor sleep is associated with sensation-seeking and risk behavior in college students. Sleep Sci. 2022 Jan-Mar;15(Spec 1):249-256. [CrossRef] [PubMed] [PubMed Central]
- Salfi, F.; Lauriola, M.; Tempesta, D.; Calanna, P.; Socci, V.; De Gennaro, L.; Ferrara, M. Effects of Total and Partial Sleep Deprivation on Reflection Impulsivity and Risk-Taking in Deliberative Decision-Making. Nat Sci Sleep. 2020; 12:309-324. 27 May. [CrossRef] [PubMed] [PubMed Central]
- https://link.springer.com/article/10.3758/s13423-024-02549-6.
- Davidson, J. D. (n.d.). The impact of sleep on academic burnout with the effects of perceived stress and general well-being. Scholarship@Western. https://ir.lib.uwo.ca/brescia_psych_uht/48/.
- Saintila, J.; Soriano-Moreno, A.N.; Ramos-Vera, C.; Oblitas-Guerrero, S.M.; Calizaya-Milla, Y.E. Association between sleep duration and burnout in healthcare professionals: a cross-sectional survey. Frontiers in Public Health 2024, 11. [Google Scholar] [CrossRef]
- Bernert, R.A. Sleep disturbances and suicide risk: A review of the literature. Neuropsychiatric Disease and Treatment 2008, 3, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, J.; McDaniel, K.; DiBlanda, A. Association between insufficient sleep, depressive symptoms, and suicidality among Florida high school students. Preventing Chronic Disease 2023, 20. [Google Scholar] [CrossRef]
- Kim, M.J.; Shin, D.; Ahn, Y.M. Association between the number of hours of sleep during weekdays and suicidality among Korean adolescents: Mediating role of depressive and anxiety symptoms. Journal of Affective Disorders 2022, 320, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Summer, J., & Summer, J. (2023, January 6). Microsleep: What is it, what causes it, and is it safe? Sleep Foundation. https://www.sleepfoundation.org/how-sleep-works/microsleep.
- Boyle, L.N.; Tippin, J.; Paul, A.; Rizzo, M. Driver performance in the moments surrounding a microsleep. Transportation Research Part F Traffic Psychology and Behaviour 2007, 11, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Hammond, C. (2024, January 31). Microsleeps: The naps that may only last seconds. https://www.bbc.com/future/article/20240130-microsleeps-the-naps-that-may-only-last-seconds.
- Wang, Y.; Guang, Z.; Zhang, J.; Han, L.; Zhang, R.; Chen, Y.; Chen, Q.; Liu, Z.; Gao, Y.; Wu, R.; Wang, S. Effect of Sleep Quality on Anxiety and Depression Symptoms among College Students in China’s Xizang Region: The Mediating Effect of Cognitive Emotion Regulation. Behavioral Sciences 2023, 13, 861. [Google Scholar] [CrossRef]
- Andishmand, Z.; Amini, A.; Naderi, F.; Garmabi, M.; Sharifnezhad, A.; Darrudi, F.; Gholami, A. Is sleep duration associated with depression and anxiety? A Cross-Sectional Study on medical students in Iran. Sleep Medicine Research 2023, 14, 200–206. [Google Scholar] [CrossRef]
- Gottlieb, D. J. , Ellenbogen, J. M., Bianchi, M. T., & Czeisler, C. A. (2018, March 20). Sleep deficiency and motor vehicle crash risk in the general population: A prospective cohort study, 20 March 5859. [Google Scholar]
- Al-Houqani, M.; Eid, H.O.; Abu-Zidan, F.M. Sleep-related collisions in United Arab Emirates. Accident Analysis & Prevention 2013, 50, 1052–1055. [Google Scholar] [CrossRef]
| Category | Variable | Percentage (n) |
|---|---|---|
| Gender | Female | 76.3% (245) |
| Male | 23.7% (76) | |
| Emirate | Dubai | 45.8% (147) |
| Sharjah | 27.4% (88) | |
| Abu Dhabi | 10.6% (34) | |
| Ajman | 7.8% (25) | |
| Fujairah | 6.5% (21) | |
| Umm Al Quwain | 0.9% (3) | |
| Ras Al Khaimah | 0.9% (3) | |
| Ethnicity | South Asia | 59.2% (190) |
| Middle East | 17.8% (57) | |
| Southeast Asia | 12.55% (40) | |
| African/Caribbean | 5% (16) | |
| East Asia | 4.4% (14) | |
| Americans | 0.9% (3) | |
| European | 0.3% (3) | |
| Age [34] (in years) | Youth (18-24) | 51.4% (165) |
| Young Adult (25-44) | 35.2% (113) | |
| Middle Age (45-65) | 13.4% (43) |
| Physical health conditions | Sleep Duration | p-value |
|---|---|---|
| Pre-diabetic/diabetes | Sleep Deprived (4) 4.21% | 0.88 |
| Adequate sleep (16) 7.07% | ||
| High Cholesterol | Sleep Deprived (3) 3.15% | |
| Adequate sleep (9) 3.98% | ||
| Hypertension | Sleep Deprived (2) 2.1% | |
| Adequate sleep (3) 1.32% | ||
| Three comorbidities | Sleep Deprived (1) 1.05% | |
| Adequate sleep (2) 0.88% | ||
| Two comorbidities | Sleep Deprived (5) 5.26% | |
| Adequate sleep (8) 3.53% | ||
| No health conditions | Sleep Deprived (80) 84.2% | |
| Adequate sleep (188) 83.1% |
| Category | Sleep duration | Frequently | Sometimes/Infrequently | P - Value |
|---|---|---|---|---|
| Sleep Duration and Forgetfulness | Sleep Deprived (95) | 24.2% (23) | 72 (75.7%) | 0.5 |
| Adequate sleep (226) | 19.0% (43) | 183 (81 %) | ||
| Sleep duration and difficulty in concentrating during daily tasks | Sleep deprived (95) | 28.4% (27) | 71.5% (68) | 0.04 |
| Adequate sleep (226) | 16.8% (38) | 83.1% (188) | ||
| Irritability/ Annoyance | Sleep Deprived (95) | 29.47% (28) | 70.5% (67) | 0.277 |
| Adequate sleep (226) | 23.4% (53) | 76.5% (173) | ||
| Decision Making | Sleep Deprived (95) |
8.7% (28) |
70.5% (67) | 0.211 |
| Adequate sleep (226) | 20.8% (47) | 79.2% (179) |
| Category | Sleep duration | Frequently | Sometimes/Infrequently | P - value |
|---|---|---|---|---|
| Engaging in risky behaviours | Sleep Deprived (95) | 5.3% (5) | 94.7% (90) | 0.539 |
| Adequate sleep (226) | 7.1% (16) | 92.9% (210) | ||
| Feelings of Depression / Hopelessness |
Sleep Deprived (95) | 22.10% (21) | 77.89% (74) | 0.016 |
| Adequate sleep (226) | 15.04% (34) | 84.95% (192) | ||
| Sleep Duration and Micro Sleep Episodes (Falling asleep while doing daily tasks) | Sleep Deprived (95) | 7.36% (7) | 92.63% (88) | 0.08 |
| Adequate sleep (226) | 4.86% (11) | 95.13% (215) |
| Feelings of Anxiety/ Nervous/ On Edge | Sleep duration | Always | Often | Sometimes | Rarely | Never | P- value |
| Sleep Deprived (95) | 7.4% (7) | 21.1% (20) |
44.2% (42) | 11.6% (11) | 15.8% (15) | 0.054 | |
| Adequate sleep (226) | 7.5% (17) | 14.2 %(32) | 37.2% (84) | 26.1% (59) | 15% (38) |
| Category | Sleep duration | Yes | No | I do not drive | P-Value |
|---|---|---|---|---|---|
| Road Traffic Accident | Sleep Deprived (95) | 5.26% (5) | 66.3% (63) | 28.42% (27) | 0.64 |
| Adequate Sleep (226) | 3.53% (8) | 70.79% (160) | 25.66% (58) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





