Submitted:
29 January 2025
Posted:
30 January 2025
Read the latest preprint version here
Abstract

Keywords:
Introduction
How Much Evidence Is Enough?
Means, Motive and Opportunity
Two Lines of Easily Misconstrued Evidence Dominate the Field
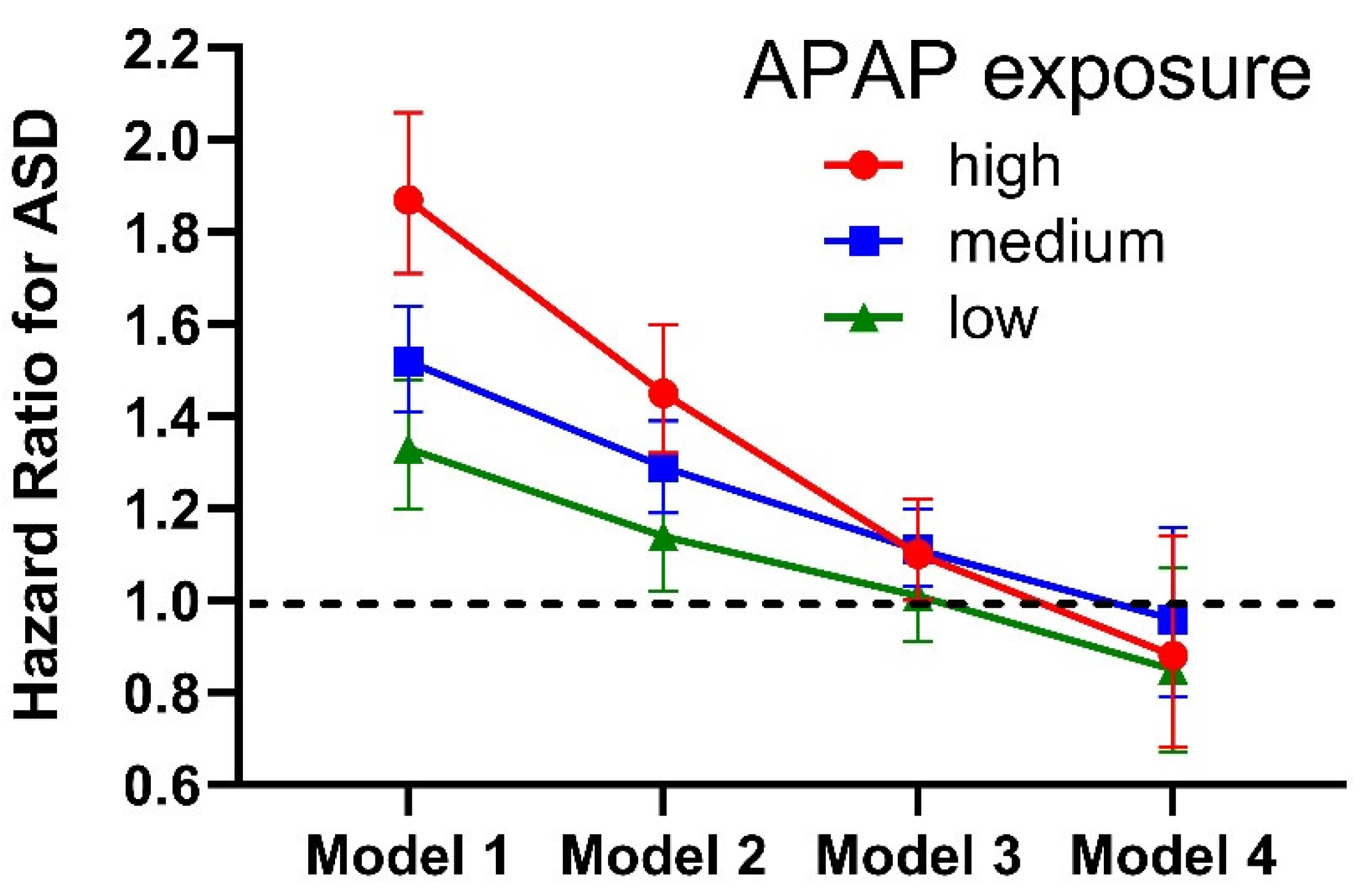
“Specifically, in utero (but not postnatal) exposure to paracetamol results in a 19% increased risk of ASD (Masarwa et al., 2018; Alemany et al., 2021; Khan et al., 2022)…”
“It is concluded that risks of acetaminophen use for neurodevelopment obtained from multivariate analysis of cohort data depend on underlying assumptions in the analyses, and that other evidence, both abundant and robust, demonstrate the critical role of acetaminophen in the etiology of ASD.”
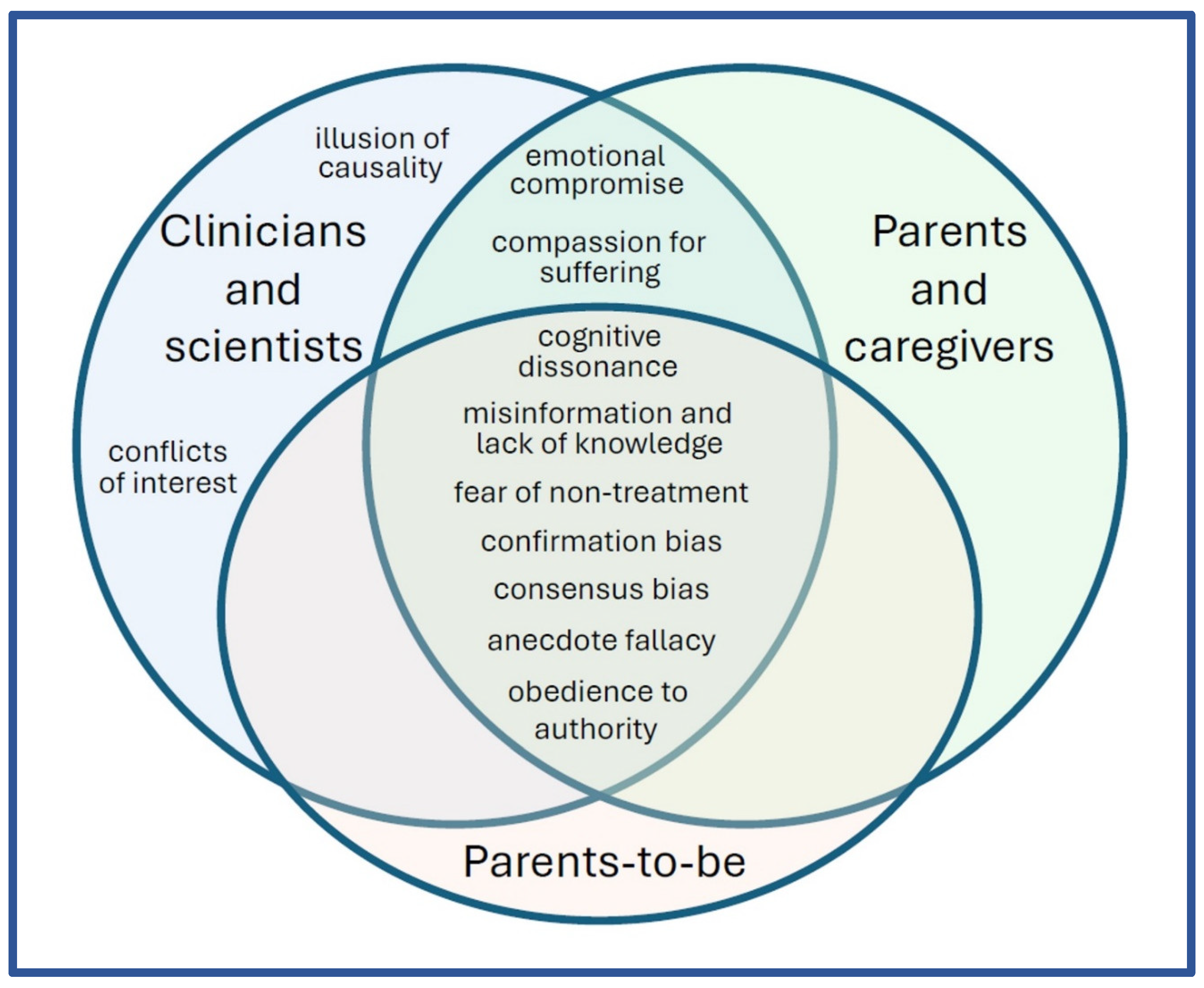
Barriers to Moving Forward
Clinical Implications
Conclusions
| Evidence / references | Background / additional information |
|---|---|
| 1. Mechanisms of APAP-mediated injury are plausible. For review, see Jones et al. [4] | The first study showing that children with ASD are deficient in a metabolic pathway necessary to safely detoxify APAP in babies (sulfation) is now more than a quarter of a century old [79], and was subsequently corroborated [80,81]. One enzyme (CyP450 2E1) which produces the toxic metabolite of APAP (NAPQI) is expressed in the human brain from before birth [82] and is a target of epigenetic alterations in mothers who have children with ASD [83]. In addition, polymorphisms in another enzyme (CyP450 1A2) that produces the same toxic metabolite of APAP is associated with ASD [84,85]. |
| 2. APAP use during early childhood is associated with a 20-fold greater risk of regressive ASD [16]. | This case-controlled study, now more than 16 years old, has been widely criticized, but careful analysis does not reveal any credible objections [1]. |
| 3. APAP use with mild adverse reactions to a vaccine, but not mild adverse reactions to a vaccine alone, is associated with ASD [16]. | This study, the same as in line of evidence #2, was the first study to separate the impact of vaccines from APAP on neurodevelopment, and the first to implicate APAP with the etiology of ASD. |
| 4. APAP was never demonstrated to be safe for neurodevelopment [17]. Over two thousand papers in the medical literature claim that APAP is safe for babies and/or children when used as directed, but all studies were based on the false assumption that adverse reactions in babies would involve easily measured liver injury, the same as in adults [17]. | Like APAP, opioids have also never been shown to be safe for neurodevelopment [86]. However, unlike APAP, opioids are not generally assumed to be safe for neurodevelopment when used as directed. Further, one study probing the safety of prenatal opioid exposure found reductions in communication skills in children associated with prenatal APAP exposure, but not with prenatal opioid exposure [39]. |
| 5. Numerous studies in laboratory animals from multiple laboratories indicate that early life exposure to APAP causes long term changes in brain function [59,87,88,89,90,91,92,93]. | After adjusting for weight, the amount of APAP that causes profound changes in laboratory animals in some studies is very close to [59] or even less than [87] the amount administered to human babies and children. Thus, APAP could never be used in babies or children if current guidelines for drug safety were applied. |
| 6. Early life exposure to APAP has a greater long-term impact on male laboratory animals than female laboratory animals [89,92,94]. ASD is more common in males than in females. | The reason or reasons why males are more susceptible to APAP-mediated injury has been considered in some detail, and several plausible mechanisms have been proposed [89,94]. |
| 7. Prenatal exposure of laboratory rats to APAP causes problems with the processing of sound [11]. Some degree of auditory dysfunction is seen in the majority of individuals with ASD. Reviewed by Graeca and Kulesza [11]. | The investigators found developmental delays with ear opening and, essentially, difficulty with hearing later in life after exposure to APAP as a fetus. It is unknown whether these affects in laboratory animals are related to impairments in some individuals with ASD. |
| 8. APAP causes apoptosis-mediated death of cortical neurons in laboratory rats [95], and cortical neurons may be involved in the pathology of ASD [96,97]. | Increased levels of biomarkers for neuronal apoptosis [98,99,100] and impaired autophagy [101] are associated with ASD. Autophagy is necessary to clearing damaged organelles such as mitochondria [102], which are created by aberrant metabolism of APAP [103]. |
| 9. Genetic, epigenetic, and environmental factors associated with an increased risk of ASD have an adverse effect on the body’s ability to safely metabolize APAP [20,79,104]. | The wide array of factors associated with ASD have led to the hypothesis that many things can come together to cause ASD, but ASD is characterized by impairment of social function and other particular behavioral phenotypes, suggesting specificity in the etiology of the condition. |
| 10. Cystic fibrosis is associated with unusually efficient (effective) metabolism of APAP [105,106], and the prevalence of ASD is apparently very low in patients with cystic fibrosis [20]. | The mental health of patients with cystic fibrosis has been characterized extensively, but no association between ASD and cystic fibrosis has been reported. |
| 11. APAP temporarily blunts social trust [107] and awareness [108], emotional responses to external stimuli [109], and the ability to identify errors [110] in adults. | Although the mechanisms are unknown, these studies show that APAP affects aspects of mental function that are impaired in individuals with ASD. |
| 12. Higher le[19,21,22,33–52vels of APAP in cord blood are associated with ASD [21]. | For the analysis, the authors divided the women into three groups based on cord blood APAP levels. The third with the highest levels had 3.6 times more likelihood of having a child with ASD that the third with the lowest levels of APAP. |
| 13. Use of APAP during pregnancy has been associated with adverse long-term effects on the mental health of offspring in numerous studies [19,21,22,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52]. | This line of evidence has received more attention than any other line of evidence, to the point of being the only line of evidence considered by many investigators. However, the numerous studies underpinning this line of evidence are hampered by several factors which can cause errors in estimation of the association between APAP and ASD [4]. A recent study found a dramatic association (odds ratio (OR) for ASD with APAP use = 1.8) [23], but incorrectly and completely cancelled out that association using an error in the assumptions underlying the statistical analysis [2,4]. |
| 14. Analysis of the Danish National Birth Cohort (DNBC) revealed an odds ratio (OR) of 1.3 (CI 1.02–1.66) for ASD associated with postnatal APAP exposure [38], despite the fact that the use of APAP appears to be dramatically underreported in the DNBC [1]. | The study authors averaged the results from the DNBC with assessments of autism-like symptoms (not ASD) from smaller data sets, and reported no association between APAP use and those symptoms (not ASD) in the abstract of the paper [38]. This issue has been addressed in detail by us in the literature [1,2], but unfortunately may still result in confusion [11]. In addition, the study [38] employed invalid statistical adjustments expected to underestimate the association between APAP and ASD [2,4]. See text for additional discussion. |
| 15. The incidence of ASD began to increase in the early 1980s, coinciding with the increase in APAP use after aspirin was associated with Reye’s syndrome [20] | Temporal associations do not prove causality, but are a necessary prerequisite for causality to exist. Alternative explanations for the rise in prevalence of ASD face several insurmountable problems, previously reviewed [1,4]. |
| 16. The incidence of ASD has steadily increased [20] as direct-to-consumer advertising [111] and perhaps other factors such as mandated use of APAP with the MenB vaccine (see discussion) have led to increased APAP exposure early in life. | Temporal associations do not prove causality, but are a necessary prerequisite for causality to exist. Alternative explanations for the rise in prevalence of ASD face several insurmountable problems, previously reviewed [1,4]. One possible explanation for the persistence of unrealistic alternative explanations may be that many investigators are unaware of a satisfactory explanation consistent with available evidence. |
| 17. The ratio of regressive to infantile ASD rose at the same time as pediatric APAP use rose [112] after aspirin was associated with Reye’s syndrome [20]. | This observation, made in 2000, would suggest that something was introduced into the environment that could induce ASD after months or even years of neurodevelopment. This factor was tragically and incorrectly suspected to be a vaccine at that time, an issue that was decisively addressed by Stephen Schultz eight years later (see line of evidence #3). |
| 18. Circumcision of males is associated with a 2-fold increase in the risk for early-onset (infantile) ASD [60]. | Circumcision is often performed using APAP as an analgesic despite the fact that such use is of highly questionable effectiveness [113]. |
| 19. The popularity of APAP use and the prevalence of ASD was substantially higher in Denmark than in Finland in the mid-2000s [3]. | Geographic-dependent associations do not prove causality, but do contribute to the total body of evidence. Particularly in the absence of alternative explanations, these associations can be compelling. |
| 20. An exceptionally high prevalence of ASD was identified in South Korea [114,115] following repeated findings of levels of APAP exceeding the package label of children’s products [116]. | Repeating mistakes made when the initial determination of APAP safety for pediatric use was determined (See line of evidence #4), public health authorities assessed the prevalence of reports of liver failure in the pediatric population, and determined that no harm was caused by the excess active ingredient (APAP) in the formulation. Liver failure is the primary adverse event from APAP overdose in adults. However, a study in laboratory animals in the 1980s demonstrated that the liver is not susceptible to APAP-mediated injury in very young animals, even with lethal doses of APAP [117]. |
| 21. Ultra-Orthodox Jews [118] in Israel have a reported prevalence of ASD less than half of that of reform Jews. Traditional circumcision practices employed by Ultra-Orthodox Jews do not utilize APAP. | Circumcision is often performed using APAP as an analgesic despite the fact that such use is of highly questionable effectiveness [113]. Almost all Israeli Jews are circumcised [119]. |
| 22. APAP is not used in domestic cats because they lack of a robust glucuronidation-dependent capacity for metabolism [120,121,122,123], making them susceptible to APAP-mediated injury. Human neonates also lack a robust glucuronidation-dependent pathway [124,125]. | Based on liver function in human babies and children, APAP was incorrectly determined to be safe for pediatric use in the 1960s and 1970s (see line of evidence # 4), before this evidence from veterinary science became available in the 1980s. One study in laboratory animals in the 1980s showed that even lethal doses of APAP do not cause liver failure in neonates [117], but the first study showing APAP-mediated neurodevelopmental brain injury in laboratory animals was not published until 2013 [59]. |
| 23. Surveys show that up to 50% of parents who have a child with ASD believe that their children’s ASD was induced by a vaccine [126,127]. | Although this belief has been widely attributed to a 1998 report describing 12 patients [128], the title of that report is not intelligible to individuals outside of the medical profession, and medical papers have seldom affected public opinion. A more likely explanation involves the induction of ASD by APAP use concurrent with vaccination, as suggested by Schultz [16,129]. |
| 24. Studies in several countries with chronic shortages of medication found dramatically lower-than-expected levels of ASD relative to other developmental issues, including Down syndrome. Reviewed by Jones et al. [4] | Not included in the previous review of this issue [4] is the apparently low levels of ASD in Cuba, where 241 cases of ASD in the entire nation (1 in 25,000 children) have been identified based on a 2016 report [130]. APAP is available in Cuba by prescription only [131], and multiple travel advisors cite APAP in particular as being in short supply in Cuba [132,133,134,135]. |
| 25. APAP binds directly to arachidonic acid [13] and affects arachidonic acid metabolism [12]. Alterations of arachidonic acid [15] and enzymes involved in arachidonic acid metabolism [14] are associated with ASD. | It is unknown what role arachidonic acid plays in ASD, but arachidonic acid plays a role in both the analgesic and antipyretic properties of APAP, and its metabolism is associated with ASD. |
| 26. The “missing heritability” paradox of ASD suggests that epigenetic factors or very early exposure to environmental factors might influence the onset of ASD [136]. | The role of APAP in the induction of ASD nicely resolves the missing heritability paradox connected with ASD, in which sibling studies indicate a high contribution of genetics, but genome wide studies fail to identify the genes involved [136]. The observation that abuse of a mother when she was a child is associated with ASD in the offspring [137] is one example of evidence that supports this view. |
| 27. ASD and fetal alcohol spectrum disorder (FASD) are similar in many regards. Reviewed by Jones et al. [4] A spectrum disorder can also be triggered by the drug valproate [5]. | These observations demonstrates that a complex spectrum disorder (FASD) sharing many similarities with ASD can (a) be induced by a single chemical and (b) be influenced by a variety of genetic and environmental factors. |
| Variable | HR (CI) | p |
|---|---|---|
| APAP, actual risk built into virtual construct | 2.667 (NA) | NA |
| APAP, result of regression analysis | 2.55 (2.41-2.71) | 2 x 10-16 |
| APAP, adjusted for all contributing cofactors | 0.85 (0.80-0.90) | 2 x 10-7 |
| OS factor 1, all individuals | 1.24 (1.23-1.26) | 2 x 10-16 |
| OS factor 1, virtual individuals with APAP use only | 1.32 (1.30-1.34) | 2 x 10-16 |
| OS factor 1, virtual individuals with no APAP use only | 1.00 (0.97-1.03) | 0.90 |
Another problem with analyses of healthcare Funding
Acknowledgements
Conflicts of Interest
References
- Zhao, L.; Jones, J.; Anderson, L.; Konsoula, Z.; Nevison, C.; Reissner, K.; Parker, W. Acetaminophen causes neurodevelopmental injury in susceptible babies and children: no valid rationale for controversy. Clinical and experimental pediatrics, 2023. [Google Scholar] [CrossRef]
- Patel, E.; Jones Iii, J.P., 3rd; Bono-Lunn, D.; Kuchibhatla, M.; Palkar, A.; Cendejas Hernandez, J.; Sarafian, J.T.; Lawton, V.G.; Anderson, L.G.; Konsoula, Z.; et al. The safety of pediatric use of paracetamol (acetaminophen): a narrative review of direct and indirect evidence. Minerva pediatrics 2022, 74, 774–788. [Google Scholar] [CrossRef] [PubMed]
- Parker, W.; Anderson, L.G.; Jones, J.P.; Anderson, R.; Williamson, L.; Bono-Lunn, D.; Konsoula, Z. The Dangers of Acetaminophen for Neurodevelopment Outweigh Scant Evidence for Long-Term Benefits. Children 2024, 11, 44. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.P., 3rd; Williamson, L.; Konsoula, Z.; Anderson, R.; Reissner, K.J.; Parker, W. Evaluating the Role of Susceptibility Inducing Cofactors and of Acetaminophen in the Etiology of Autism Spectrum Disorder. Life (Basel, Switzerland) 2024, 14. [Google Scholar] [CrossRef] [PubMed]
- Clayton-Smith, J.; Bromley, R.; Dean, J.; Journel, H.; Odent, S.; Wood, A.; Williams, J.; Cuthbert, V.; Hackett, L.; Aslam, N.; et al. Diagnosis and management of individuals with Fetal Valproate Spectrum Disorder; a consensus statement from the European Reference Network for Congenital Malformations and Intellectual Disability. Orphanet journal of rare diseases 2019, 14, 180. [Google Scholar] [CrossRef]
- Albano, E.; Rundgren, M.; Harvison, P.J.; Nelson, S.D.; Moldéus, P. Mechanisms of N-acetyl-p-benzoquinone imine cytotoxicity. Mol. Pharmacol. 1985, 28, 306–311. [Google Scholar] [CrossRef]
- Luo, G.; Huang, L.; Zhang, Z. The molecular mechanisms of acetaminophen-induced hepatotoxicity and its potential therapeutic targets. Exp. Biol. Med. (Maywood) 2023, 248, 412–424. [Google Scholar] [CrossRef]
- Zakhari, S. Overview: how is alcohol metabolized by the body? Alcohol research & health : the journal of the National Institute on Alcohol Abuse and Alcoholism 2006, 29, 245–254. [Google Scholar]
- LoPachin, R.M.; Gavin, T. Molecular mechanisms of aldehyde toxicity: a chemical perspective. Chem. Res. Toxicol. 2014, 27, 1081–1091. [Google Scholar] [CrossRef]
- Shnayder, N.A.; Grechkina, V.V.; Khasanova, A.K.; Bochanova, E.N.; Dontceva, E.A.; Petrova, M.M.; Asadullin, A.R.; Shipulin, G.A.; Altynbekov, K.S.; Al-Zamil, M.; et al. Therapeutic and Toxic Effects of Valproic Acid Metabolites. Metabolites 2023, 13. [Google Scholar] [CrossRef]
- Graeca, M.; Kulesza, R. Impaired brainstem auditory evoked potentials after in utero exposure to high dose paracetamol exposure. Hear. Res. 2024, 454, 109149. [Google Scholar] [CrossRef]
- Hinz, B.; Cheremina, O.; Brune, K. Acetaminophen (paracetamol) is a selective cyclooxygenase-2 inhibitor in man. FASEB J. 2008, 22, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Hogestatt, E.D.; Jonsson, B.A.; Ermund, A.; Andersson, D.A.; Bjork, H.; Alexander, J.P.; Cravatt, B.F.; Basbaum, A.I.; Zygmunt, P.M. Conversion of acetaminophen to the bioactive N-acylphenolamine AM404 via fatty acid amide hydrolase-dependent arachidonic acid conjugation in the nervous system. J. Biol. Chem. 2005, 280, 31405–31412. [Google Scholar] [CrossRef] [PubMed]
- El-Ansary, A.; Alfawaz, H.A.; Bacha, A.B.; Al-Ayadhi, L.Y. Combining Anti-Mitochondrial Antibodies, Anti-Histone, and PLA2/COX Biomarkers to Increase Their Diagnostic Accuracy for Autism Spectrum Disorders. Brain Sci 2024, 14, 576. [Google Scholar] [CrossRef] [PubMed]
- Hirai, T.; Umeda, N.; Harada, T.; Okumura, A.; Nakayasu, C.; Ohto-Nakanishi, T.; Tsuchiya, K.J.; Nishimura, T.; Matsuzaki, H. Arachidonic acid-derived dihydroxy fatty acids in neonatal cord blood relate symptoms of autism spectrum disorders and social adaptive functioning: Hamamatsu Birth Cohort for Mothers and Children (HBC Study). Psychiatry and clinical neurosciences 2024, 78, 546–557. [Google Scholar] [CrossRef]
- Schultz, S.T.; Klonoff-Cohen, H.S.; Wingard, D.L.; Akshoomoff, N.A.; Macera, C.A.; Ji, M. Acetaminophen (paracetamol) use, measles-mumps-rubella vaccination, and autistic disorder. The results of a parent survey. Autism 2008, 12, 293–307. [Google Scholar] [CrossRef]
- Cendejas-Hernandez, J.; Sarafian, J.; Lawton, V.; Palkar, A.; Anderson, L.; Lariviere, V.; Parker, W. Paracetamol (Acetaminophen) Use in Infants and Children was Never Shown to be Safe for Neurodevelopment: A Systematic Review with Citation Tracking. Eur. J. Pediatr. 2022, 181, 1835–1857. [Google Scholar] [CrossRef]
- Ertmann, R.K.; Møller, J.J.; Waldorff, F.B.; Siersma, V.; Reventlow, S.; Söderström, M. The majority of sick children receive paracetamol during the winter. Danish medical journal 2012, 59, A4555. [Google Scholar]
- Bornehag, C.G.; Reichenberg, A.; Hallerback, M.U.; Wikstrom, S.; Koch, H.M.; Jonsson, B.A.; Swan, S.H. Prenatal exposure to acetaminophen and children's language development at 30 months. Eur. Psychiatry 2018, 51, 98–103. [Google Scholar] [CrossRef]
- Parker, W.; Hornik, C.D.; Bilbo, S.; Holzknecht, Z.E.; Gentry, L.; Rao, R.; Lin, S.S.; Herbert, M.R.; Nevison, C.D. The role of oxidative stress, inflammation and acetaminophen exposure from birth to early childhood in the induction of autism. J. Int. Med. Res. 2017, 45, 407–438. [Google Scholar] [CrossRef]
- Ji, Y.; Azuine, R.E.; Zhang, Y.; Hou, W.; Hong, X.; Wang, G.; Riley, A.; Pearson, C.; Zuckerman, B.; Wang, X. Association of Cord Plasma Biomarkers of In Utero Acetaminophen Exposure With Risk of Attention-Deficit/Hyperactivity Disorder and Autism Spectrum Disorder in Childhood. JAMA Psychiatry 2020, 77, 180–189. [Google Scholar] [CrossRef]
- Baker, B.H.; Lugo-Candelas, C.; Wu, H.; Laue, H.E.; Boivin, A.; Gillet, V.; Aw, N.; Rahman, T.; Lepage, J.F.; Whittingstall, K.; et al. Association of Prenatal Acetaminophen Exposure Measured in Meconium With Risk of Attention-Deficit/Hyperactivity Disorder Mediated by Frontoparietal Network Brain Connectivity. JAMA pediatrics 2020, 174, 1073–1081. [Google Scholar] [CrossRef] [PubMed]
- Ahlqvist, V.H.; Sjöqvist, H.; Dalman, C.; Karlsson, H.; Stephansson, O.; Johansson, S.; Magnusson, C.; Gardner, R.M.; Lee, B.K. Acetaminophen Use During Pregnancy and Children's Risk of Autism, ADHD, and Intellectual Disability. Jama 2024, 331, 1205–1214. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, V. Study reveals no causal link between neurodevelopmental disorders and acetaminophen exposure before birth. NIH: 2024.
- Lexchin, J.; Bero, L.A.; Djulbegovic, B.; Clark, O. Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ 2003, 326, 1167–1170. [Google Scholar] [CrossRef] [PubMed]
- Lundh, A.; Lexchin, J.; Mintzes, B.; Schroll, J.B.; Bero, L. Industry sponsorship and research outcome. Cochrane Database Syst Rev 2017, 2, Mr000033. [Google Scholar] [CrossRef]
- Bero, L.; Oostvogel, F.; Bacchetti, P.; Lee, K. Factors associated with findings of published trials of drug-drug comparisons: why some statins appear more efficacious than others. PLoS Med 2007, 4, e184. [Google Scholar] [CrossRef]
- Bero, L.A. Tobacco industry manipulation of research. Public health reports (Washington, D.C. : 1974) 2005, 120, 200–208. [Google Scholar] [CrossRef]
- Fabbri, A.; Holland, T.J.; Bero, L.A. Food industry sponsorship of academic research: investigating commercial bias in the research agenda. Public health nutrition 2018, 21, 3422–3430. [Google Scholar] [CrossRef]
- Whitstock, M. Manufacturing the truth: From designing clinical trials to publishing trial data. Indian journal of medical ethics 2018, 3, 152–162. [Google Scholar] [CrossRef]
- Gupta, R.; Chernesky, J.; Lembke, A.; Michaels, D.; Tomori, C.; Greene, J.A.; Alexander, G.C.; Koon, A.D. The opioid industry's use of scientific evidence to advance claims about prescription opioid safety and effectiveness. Health affairs scholar 2024, 2, qxae119. [Google Scholar] [CrossRef]
- Legg, T.; Hatchard, J.; Gilmore, A.B. The Science for Profit Model-How and why corporations influence science and the use of science in policy and practice. PLoS One 2021, 16, e0253272. [Google Scholar] [CrossRef]
- Tovo-Rodrigues, L.; Schneider, B.C.; Martins-Silva, T.; Del-Ponte, B.; Loret de Mola, C.; Schuler-Faccini, L.; Vianna, F.S.L.; Munhoz, T.N.; Entiauspe, L.; Silveira, M.F.; et al. Is intrauterine exposure to acetaminophen associated with emotional and hyperactivity problems during childhood? Findings from the 2004 Pelotas birth cohort. BMC Psychiatry 2018, 18, 368. [Google Scholar] [CrossRef] [PubMed]
- Vlenterie, R.; Wood, M.E.; Brandlistuen, R.E.; Roeleveld, N.; van Gelder, M.M.; Nordeng, H. Neurodevelopmental problems at 18 months among children exposed to paracetamol in utero: a propensity score matched cohort study. Int. J. Epidemiol. 2016, 45, 1998–2008. [Google Scholar] [CrossRef] [PubMed]
- Liew, Z.; Ritz, B.; Virk, J.; Arah, O.A.; Olsen, J. Prenatal Use of Acetaminophen and Child IQ: A Danish Cohort Study. Epidemiology 2016, 27, 912–918. [Google Scholar] [CrossRef]
- Liew, Z.; Bach, C.C.; Asarnow, R.F.; Ritz, B.; Olsen, J. Paracetamol use during pregnancy and attention and executive function in offspring at age 5 years. Int. J. Epidemiol. 2016, 45, 2009–2017. [Google Scholar] [CrossRef]
- Avella-Garcia, C.B.; Julvez, J.; Fortuny, J.; Rebordosa, C.; Garcia-Esteban, R.; Galan, I.R.; Tardon, A.; Rodriguez-Bernal, C.L.; Iniguez, C.; Andiarena, A.; et al. Acetaminophen use in pregnancy and neurodevelopment: attention function and autism spectrum symptoms. Int. J. Epidemiol. 2016, 45, 1987–1996. [Google Scholar] [CrossRef]
- Alemany, S.; Avella-García, C.; Liew, Z.; García-Esteban, R.; Inoue, K.; Cadman, T.; López-Vicente, M.; González, L.; Riaño Galán, I.; Andiarena, A.; et al. Prenatal and postnatal exposure to acetaminophen in relation to autism spectrum and attention-deficit and hyperactivity symptoms in childhood: Meta-analysis in six European population-based cohorts. Eur. J. Epidemiol. 2021, 36, 993–1004. [Google Scholar] [CrossRef]
- Skovlund, E.; Handal, M.; Selmer, R.; Brandlistuen, R.E.; Skurtveit, S. Language competence and communication skills in 3-year-old children after prenatal exposure to analgesic opioids. Pharmacoepidemiol. Drug Saf. 2017, 26, 625–634. [Google Scholar] [CrossRef]
- Liew, Z.; Ritz, B.; Rebordosa, C.; Lee, P.C.; Olsen, J. Acetaminophen use during pregnancy, behavioral problems, and hyperkinetic disorders. JAMA pediatrics 2014, 168, 313–320. [Google Scholar] [CrossRef]
- Liew, Z.; Ritz, B.; Virk, J.; Olsen, J. Maternal use of acetaminophen during pregnancy and risk of autism spectrum disorders in childhood: A Danish national birth cohort study. Autism research : official journal of the International Society for Autism Research 2016, 9, 951–958. [Google Scholar] [CrossRef]
- Ystrom, E.; Gustavson, K.; Brandlistuen, R.E.; Knudsen, G.P.; Magnus, P.; Susser, E.; Davey Smith, G.; Stoltenberg, C.; Suren, P.; Haberg, S.E.; et al. Prenatal Exposure to Acetaminophen and Risk of ADHD. Pediatrics 2017, 140. [Google Scholar] [CrossRef]
- Thompson, J.M.; Waldie, K.E.; Wall, C.R.; Murphy, R.; Mitchell, E.A. Associations between acetaminophen use during pregnancy and ADHD symptoms measured at ages 7 and 11 years. PLoS One 2014, 9, e108210. [Google Scholar] [CrossRef] [PubMed]
- Stergiakouli, E.; Thapar, A.; Davey Smith, G. Association of Acetaminophen Use During Pregnancy With Behavioral Problems in Childhood: Evidence Against Confounding. JAMA pediatrics 2016, 170, 964–970. [Google Scholar] [CrossRef] [PubMed]
- Brandlistuen, R.E.; Ystrom, E.; Nulman, I.; Koren, G.; Nordeng, H. Prenatal paracetamol exposure and child neurodevelopment: a sibling-controlled cohort study. Int. J. Epidemiol. 2013, 42, 1702–1713. [Google Scholar] [CrossRef] [PubMed]
- Sznajder, K.K.; Teti, D.M.; Kjerulff, K.H. Maternal use of acetaminophen during pregnancy and neurobehavioral problems in offspring at 3 years: A prospective cohort study. PLoS One 2022, 17, e0272593. [Google Scholar] [CrossRef]
- Inoue, K.; Ritz, B.; Ernst, A.; Tseng, W.L.; Yuan, Y.; Meng, Q.; Ramlau-Hansen, C.H.; Strandberg-Larsen, K.; Arah, O.A.; Obel, C.; et al. Behavioral Problems at Age 11 Years After Prenatal and Postnatal Exposure to Acetaminophen: Parent-Reported and Self-Reported Outcomes. Am. J. Epidemiol. 2021, 190, 1009–1020. [Google Scholar] [CrossRef]
- Liew, Z.; Kioumourtzoglou, M.A.; Roberts, A.L.; O'Reilly É, J.; Ascherio, A.; Weisskopf, M.G. Use of Negative Control Exposure Analysis to Evaluate Confounding: An Example of Acetaminophen Exposure and Attention-Deficit/Hyperactivity Disorder in Nurses' Health Study II. Am. J. Epidemiol. 2019, 188, 768–775. [Google Scholar] [CrossRef]
- Parker, S.E.; Collett, B.R.; Werler, M.M. Maternal acetaminophen use during pregnancy and childhood behavioural problems: Discrepancies between mother- and teacher-reported outcomes. Paediatr Perinat Epidemiol 2020, 34, 299–308. [Google Scholar] [CrossRef]
- Trønnes, J.N.; Wood, M.; Lupattelli, A.; Ystrom, E.; Nordeng, H. Prenatal paracetamol exposure and neurodevelopmental outcomes in preschool-aged children. Paediatr Perinat Epidemiol 2020, 34, 247–256. [Google Scholar] [CrossRef]
- Golding, J.; Gregory, S.; Clark, R.; Ellis, G.; Iles-Caven, Y.; Northstone, K. Associations between paracetamol (acetaminophen) intake between 18 and 32 weeks gestation and neurocognitive outcomes in the child: A longitudinal cohort study. Paediatr Perinat Epidemiol 2020, 34, 257–266. [Google Scholar] [CrossRef]
- Chen, M.H.; Pan, T.L.; Wang, P.W.; Hsu, J.W.; Huang, K.L.; Su, T.P.; Li, C.T.; Lin, W.C.; Tsai, S.J.; Chen, T.J.; et al. Prenatal Exposure to Acetaminophen and the Risk of Attention-Deficit/Hyperactivity Disorder: A Nationwide Study in Taiwan. J. Clin. Psychiatry 2019, 80. [Google Scholar] [CrossRef]
- Tovo-Rodrigues, L.; Carpena, M.X.; Martins-Silva, T.; Santos, I.S.; Anselmi, L.; Barros, A.J.D.; Barros, F.C.; Bertoldi, A.D.; Matijasevich, A. Low neurodevelopmental performance and behavioural/emotional problems at 24 and 48 months in Brazilian children exposed to acetaminophen during foetal development. Paediatr Perinat Epidemiol 2020, 34, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Masarwa, R.; Levine, H.; Gorelik, E.; Reif, S.; Perlman, A.; Matok, I. Prenatal Exposure to Acetaminophen and Risk for Attention Deficit Hyperactivity Disorder and Autistic Spectrum Disorder: A Systematic Review, Meta-Analysis, and Meta-Regression Analysis of Cohort Studies. Am. J. Epidemiol. 2018, 187, 1817–1827. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.Y.; Kabiraj, G.; Ahmed, M.A.; Adam, M.; Mannuru, S.P.; Ramesh, V.; Shahzad, A.; Chaduvula, P.; Khan, S. A Systematic Review of the Link Between Autism Spectrum Disorder and Acetaminophen: A Mystery to Resolve. Cureus 2022, 14, e26995. [Google Scholar] [CrossRef]
- Amaral, D.G. Examining the Causes of Autism. Cerebrum : the Dana forum on brain science 2017, 2017. [Google Scholar]
- Hansen, H.V. Committing Fallacies and the Appearance Condition. Argumentation 2023, 37, 253–267. [Google Scholar] [CrossRef]
- Matute, H.; Blanco, F.; Yarritu, I.; Díaz-Lago, M.; Vadillo, M.A.; Barberia, I. Illusions of causality: how they bias our everyday thinking and how they could be reduced. Frontiers in psychology 2015, 6, 888. [Google Scholar] [CrossRef]
- Viberg, H.; Eriksson, P.; Gordh, T.; Fredriksson, A. Paracetamol (Acetaminophen) Administration During Neonatal Brain Development Affects Cognitive Function and Alters Its Analgesic and Anxiolytic Response in Adult Male Mice. Toxicol. Sci. 2013, 138, 139–147. [Google Scholar] [CrossRef]
- Frisch, M.; Simonsen, J. Ritual circumcision and risk of autism spectrum disorder in 0- to 9-year-old boys: national cohort study in Denmark. J R Soc Med 2015, 108, 266–279. [Google Scholar] [CrossRef]
- Bauer, A.; Kriebel, D. Prenatal and perinatal analgesic exposure and autism: an ecological link. Environmental Health 2013, 12, 41. [Google Scholar] [CrossRef]
- Morris, B.J.; Krieger, J.N.; Klausner, J.D. CDC's Male Circumcision Recommendations Represent a Key Public Health Measure. Global health, science and practice 2017, 5, 15–27. [Google Scholar] [CrossRef]
- Sneppen, I.; Thorup, J. Foreskin Morbidity in Uncircumcised Males. Pediatrics 2016, 137. [Google Scholar] [CrossRef] [PubMed]
- Rumack, B.H. Aspirin versus acetaminophen: a comparative view. Pediatrics 1978, 62, 943–946. [Google Scholar] [PubMed]
- Chen, L.; Zhang, M.; Yung, J.; Chen, J.; McNair, C.; Lee, K.S. Safety of Rectal Administration of Acetaminophen in Neonates. The Canadian journal of hospital pharmacy 2018, 71, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.J.; van Lingen, R.A.; Hansen, T.G.; Lin, Y.C.; Holford, N.H. Acetaminophen developmental pharmacokinetics in premature neonates and infants: a pooled population analysis. Anesthesiology 2002, 96, 1336–1345. [Google Scholar] [CrossRef] [PubMed]
- Birmingham, P.K.; Tobin, M.J.; Fisher, D.M.; Henthorn, T.K.; Hall, S.C.; Coté, C.J. Initial and subsequent dosing of rectal acetaminophen in children: a 24-hour pharmacokinetic study of new dose recommendations. Anesthesiology 2001, 94, 385–389. [Google Scholar] [CrossRef]
- Montgomery, C.J.; McCormack, J.P.; Reichert, C.C.; Marsland, C.P. Plasma concentrations after high-dose (45 mg.kg-1) rectal acetaminophen in children. Canadian journal of anaesthesia = Journal canadien d'anesthesie 1995, 42, 982–986. [Google Scholar] [CrossRef]
- Coulthard, K.P.; Nielson, H.W.; Schroder, M.; Covino, A.; Matthews, N.T.; Murray, R.S.; Van Der Walt, J.H. Relative bioavailability and plasma paracetamol profiles of Panadol suppositories in children. J Paediatr Child Health 1998, 34, 425–431. [Google Scholar] [CrossRef]
- Paracetamol use with Bexsero. New Zealand: Immunisation Advisory Centre; 2018. Availabe online: https://www.immune.org.nz/factsheets/paracetamol-use-with-bexsero-r. (accessed on 21 December 2024).
- Meningococcal disease. Care, H.a.A., Ed. Australian Government: 2024.
- Using paracetamol to prevent and treat fever after MenB vaccination. Agency, U.H.S., Ed. National Health Service: UK, 2022.
- Meningococcal vaccines: Canadian Immunization Guide. Canada, P.H.A.o., Ed. Government of Canada: 2024.
- Vaccines for Children. Israel: Ministry of Health; 2021. Availabe online: https://www.gov.il/en/pages/vaccines-for-children-pamphlet. (accessed on 21 December 2024).
- Significant events in meningococcal vaccination practice in Australia. Australia: National Centre for Immunisation Research and Surveillance; 2020. Availabe online: https://www.ncirs.org.au/sites/default/files/2020-07/Meningococcal-history-July%202020.pdf. (accessed on 21 December 2024).
- Autism in Australia, 2022. Availabe online: https://www.abs.gov.au/articles/autism-australia-2022.
- Dinstein, I.; Solomon, S.; Zats, M.; Shusel, R.; Lottner, R.; Gershon, B.B.; Meiri, G.; Menashe, I.; Shmueli, D. Large increase in ASD prevalence in Israel between 2017 and 2021. Autism research : official journal of the International Society for Autism Research 2024, 17, 410–418. [Google Scholar] [CrossRef]
- O'Ryan, M.L.; Saxena, S.; Baum, F. Time for a revolution in academic medicine? BMJ 2024, 387, q2508. [Google Scholar] [CrossRef]
- Alberti, A.; Pirrone, P.; Elia, M.; Waring, R.H.; Romano, C. Sulphation deficit in "low-functioning" autistic children: a pilot study. Biol. Psychiatry 1999, 46, 420–424. [Google Scholar] [CrossRef]
- Geier, D.A.; Kern, J.K.; Garver, C.R.; Adams, J.B.; Audhya, T.; Geier, M.R. A prospective study of transsulfuration biomarkers in autistic disorders. Neurochem. Res. 2009, 34, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Pagan, C.; Benabou, M.; Leblond, C.; Cliquet, F.; Mathieu, A.; Lemière, N.; Goubran-Botros, H.; Delorme, R.; Leboyer, M.; Callebert, J.; et al. Decreased phenol sulfotransferase activities associated with hyperserotonemia in autism spectrum disorders. Translational Psychiatry 2021, 11, 23. [Google Scholar] [CrossRef] [PubMed]
- Brzezinski, M.R.; Boutelet-Bochan, H.; Person, R.E.; Fantel, A.G.; Juchau, M.R. Catalytic activity and quantitation of cytochrome P-450 2E1 in prenatal human brain. J. Pharmacol. Exp. Ther. 1999, 289, 1648–1653. [Google Scholar] [CrossRef]
- Zhu, Y.; Mordaunt, C.E.; Yasui, D.H.; Marathe, R.; Coulson, R.L.; Dunaway, K.W.; Jianu, J.M.; Walker, C.K.; Ozonoff, S.; Hertz-Picciotto, I.; et al. Placental DNA methylation levels at CYP2E1 and IRS2 are associated with child outcome in a prospective autism study. Hum. Mol. Genet. 2019, 28, 2659–2674. [Google Scholar] [CrossRef]
- Santos, J.X.; Rasga, C.; Marques, A.R.; Martiniano, H.; Asif, M.; Vilela, J.; Oliveira, G.; Sousa, L.; Nunes, A.; Vicente, A.M. A Role for Gene-Environment Interactions in Autism Spectrum Disorder Is Supported by Variants in Genes Regulating the Effects of Exposure to Xenobiotics. Frontiers in neuroscience 2022, 16, 862315. [Google Scholar] [CrossRef]
- Braam, W.; Keijzer, H.; Struijker Boudier, H.; Didden, R.; Smits, M.; Curfs, L. CYP1A2 polymorphisms in slow melatonin metabolisers: a possible relationship with autism spectrum disorder? J. Intellect. Disabil. Res. 2013, 57, 993–1000. [Google Scholar] [CrossRef]
- Kinoshita, M.; Stempel, K.S.; Borges do Nascimento, I.J.; Bruschettini, M. Systemic opioids versus other analgesics and sedatives for postoperative pain in neonates. Cochrane Database Syst Rev 2023, 3, Cd014876. [Google Scholar] [CrossRef]
- Suda, N.; Hernandez, J.C.; Poulton, J.; Jones, J.P.; Konsoula, Z.; Smith, C.; Parker, W. Therapeutic doses of paracetamol with co-administration of cysteine and mannitol during early development result in long term behavioral changes in laboratory rats. PLoS One 2020, 16, e0253543. [Google Scholar] [CrossRef]
- Philippot, G.; Gordh, T.; Fredriksson, A.; Viberg, H. Adult neurobehavioral alterations in male and female mice following developmental exposure to paracetamol (acetaminophen): characterization of a critical period. J. Appl. Toxicol. 2017, 37, 1174–1181. [Google Scholar] [CrossRef]
- Dean, S.L.; Knutson, J.F.; Krebs-Kraft, D.L.; McCarthy, M.M. Prostaglandin E2 is an endogenous modulator of cerebellar development and complex behavior during a sensitive postnatal period. Eur. J. Neurosci. 2012, 35, 1218–1229. [Google Scholar] [CrossRef]
- Philippot, G.; Hosseini, K.; Yakub, A.; Mhajar, Y.; Hamid, M.; Buratovic, S.; Fredriksson, R. Paracetamol (Acetaminophen) and its Effect on the Developing Mouse Brain. Frontiers in toxicology 2022, 4, 867748. [Google Scholar] [CrossRef] [PubMed]
- Klein, R.M.; Rigobello, C.; Vidigal, C.B.; Moura, K.F.; Barbosa, D.S.; Gerardin, D.C.C.; Ceravolo, G.S.; Moreira, E.G. Gestational exposure to paracetamol in rats induces neurofunctional alterations in the progeny. Neurotoxicol. Teratol. 2020, 77, 106838. [Google Scholar] [CrossRef] [PubMed]
- Baker, B.H.; Rafikian, E.E.; Hamblin, P.B.; Strait, M.D.; Yang, M.; Pearson, B.L. Sex-specific neurobehavioral and prefrontal cortex gene expression alterations following developmental acetaminophen exposure in mice. Neurobiol. Dis. 2023, 177, 105970. [Google Scholar] [CrossRef] [PubMed]
- Blecharz-Klin, K.; Wawer, A.; Jawna-Zboińska, K.; Pyrzanowska, J.; Piechal, A.; Mirowska-Guzel, D.; Widy-Tyszkiewicz, E. Early paracetamol exposure decreases brain-derived neurotrophic factor (BDNF) in striatum and affects social behaviour and exploration in rats. Pharmacol. Biochem. Behav. 2018, 168, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Kanno, S.I.; Tomizawa, A.; Yomogida, S.; Hara, A. Glutathione peroxidase 3 is a protective factor against acetaminophen-induced hepatotoxicity in vivo and in vitro. Int. J. Mol. Med. 2017, 40, 748–754. [Google Scholar] [CrossRef]
- Posadas, I.; Santos, P.; Blanco, A.; Muñoz-Fernández, M.; Ceña, V. Acetaminophen induces apoptosis in rat cortical neurons. PLoS One 2010, 5, e15360. [Google Scholar] [CrossRef]
- Donovan, A.P.; Basson, M.A. The neuroanatomy of autism - a developmental perspective. J. Anat. 2017, 230, 4–15. [Google Scholar] [CrossRef]
- Casanova, M.F.; Sokhadze, E.M.; Casanova, E.L.; Opris, I.; Abujadi, C.; Marcolin, M.A.; Li, X. Translational Neuroscience in Autism: From Neuropathology to Transcranial Magnetic Stimulation Therapies. The Psychiatric clinics of North America 2020, 43, 229–248. [Google Scholar] [CrossRef]
- Dong, D.; Zielke, H.R.; Yeh, D.; Yang, P. Cellular stress and apoptosis contribute to the pathogenesis of autism spectrum disorder. Autism research : official journal of the International Society for Autism Research 2018, 11, 1076–1090. [Google Scholar] [CrossRef]
- Lv, M.N.; Zhang, H.; Shu, Y.; Chen, S.; Hu, Y.Y.; Zhou, M. The neonatal levels of TSB, NSE and CK-BB in autism spectrum disorder from Southern China. Translational neuroscience 2016, 7, 6–11. [Google Scholar] [CrossRef]
- Stancioiu, F.; Bogdan, R.; Dumitrescu, R. Neuron-Specific Enolase (NSE) as a Biomarker for Autistic Spectrum Disease (ASD). Life (Basel, Switzerland) 2023, 13. [Google Scholar] [CrossRef] [PubMed]
- Ham, A.; Chang, A.Y.; Li, H.; Bain, J.M.; Goldman, J.E.; Sulzer, D.; Veenstra-VanderWeele, J.; Tang, G. Impaired macroautophagy confers substantial risk for intellectual disability in children with autism spectrum disorders. Mol. Psychiatry, 1038. [Google Scholar] [CrossRef]
- Glick, D.; Barth, S.; Macleod, K.F. Autophagy: cellular and molecular mechanisms. J. Pathol. 2010, 221, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Du, K.; Farhood, A.; Jaeschke, H. Mitochondria-targeted antioxidant Mito-Tempo protects against acetaminophen hepatotoxicity. Arch. Toxicol. 2017, 91, 761–773. [Google Scholar] [CrossRef] [PubMed]
- Frye, R.E.; Sequeira, J.M.; Quadros, E.V.; James, S.J.; Rossignol, D.A. Cerebral folate receptor autoantibodies in autism spectrum disorder. Mol. Psychiatry 2013, 18, 369–381. [Google Scholar] [CrossRef]
- Hutabarat, R.M.; Unadkat, J.D.; Kushmerick, P.; Aitken, M.L.; Slattery, J.T.; Smith, A.L. Disposition of drugs in cystic fibrosis. III. Acetaminophen. Clin. Pharmacol. Ther. 1991, 50, 695–701. [Google Scholar] [CrossRef]
- Kearns, G.L. Hepatic drug metabolism in cystic fibrosis: recent developments and future directions. Ann. Pharmacother. 1993, 27, 74–79. [Google Scholar] [CrossRef]
- Roberts, I.D.; Krajbich, I.; Way, B.M. Acetaminophen influences social and economic trust. Scientific Reports 2019, 9, 4060. [Google Scholar] [CrossRef]
- Dewall, C.N.; Macdonald, G.; Webster, G.D.; Masten, C.L.; Baumeister, R.F.; Powell, C.; Combs, D.; Schurtz, D.R.; Stillman, T.F.; Tice, D.M.; et al. Acetaminophen reduces social pain: behavioral and neural evidence. Psychol Sci 2010, 21, 931–937. [Google Scholar] [CrossRef]
- Durso, G.R.O.; Luttrell, A.; Way, B.M. Over-the-Counter Relief From Pains and Pleasures Alike: Acetaminophen Blunts Evaluation Sensitivity to Both Negative and Positive Stimuli. Psychol Sci 2015, 26, 750–758. [Google Scholar] [CrossRef]
- Randles, D.; Kam, J.W.Y.; Heine, S.J.; Inzlicht, M.; Handy, T.C. Acetaminophen attenuates error evaluation in cortex. Social Cognitive and Affective Neuroscience 2016, 11, 899–906. [Google Scholar] [CrossRef]
- Donohue, J. A history of drug advertising: the evolving roles of consumers and consumer protection. Milbank Q 2006, 84, 659–699. [Google Scholar] [CrossRef]
- Rimland, B. The autism increase: research needed on the vaccine connection. Autism Research Review International 2000.
- Howard, C.R.; Howard, F.M.; Weitzman, M.L. Acetaminophen analgesia in neonatal circumcision: the effect on pain. Pediatrics 1994, 93, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Leventhal, B.L.; Koh, Y.J.; Fombonne, E.; Laska, E.; Lim, E.C.; Cheon, K.A.; Kim, S.J.; Kim, Y.K.; Lee, H.; et al. Prevalence of autism spectrum disorders in a total population sample. Am. J. Psychiatry 2011, 168, 904–912. [Google Scholar] [CrossRef]
- Baird, G. 2.64% of South Korean children aged 7 to 12 have autism spectrum disorders. Evidence Based Mental Health 2012, 15, 11. [Google Scholar] [CrossRef]
- Hall, C.; Smith, M. Increased cGMP enforcement has gone international: South Korean action against Johnson & Johnson serves as warning. White Collar Watch 2013, June. [Google Scholar]
- Green, M.D.; Shires, T.K.; Fischer, L.J. Hepatotoxicity of acetaminophen in neonatal and young rats. I. Age-related changes in susceptibility. Toxicol. Appl. Pharmacol. 1984, 74, 116–124. [Google Scholar] [CrossRef]
- Raz, R.; Weisskopf, M.G.; Davidovitch, M.; Pinto, O.; Levine, H. Differences in autism spectrum disorders incidence by sub-populations in Israel 1992-2009: a total population study. J. Autism Dev. Disord. 2015, 45, 1062–1069. [Google Scholar] [CrossRef]
- Kacker, S.; Tobian, A.A. Male circumcision: integrating tradition and medical evidence. The Israel Medical Association journal : IMAJ 2013, 15, 37–38. [Google Scholar]
- Anvik, J.O. Acetaminophen toxicosis in a cat. The Canadian veterinary journal = La revue veterinaire canadienne 1984, 25, 445–447. [Google Scholar]
- Savides, M.C.; Oehme, F.W.; Nash, S.L.; Leipold, H.W. The toxicity and biotransformation of single doses of acetaminophen in dogs and cats. Toxicol. Appl. Pharmacol. 1984, 74, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Court, M.H. Feline drug metabolism and disposition: pharmacokinetic evidence for species differences and molecular mechanisms. The Veterinary clinics of North America. Small animal practice 2013, 43, 1039–1054. [Google Scholar] [CrossRef]
- Lautz, L.S.; Jeddi, M.Z.; Girolami, F.; Nebbia, C.; Dorne, J. Metabolism and pharmacokinetics of pharmaceuticals in cats (Felix sylvestris catus) and implications for the risk assessment of feed additives and contaminants. Toxicology letters 2021, 338, 114–127. [Google Scholar] [CrossRef]
- Miller, R.P.; Roberts, R.J.; Fischer, L.J. Acetaminophen elimination kinetics in neonates, children, and adults. Clin. Pharmacol. Ther. 1976, 19, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Cook, S.F.; Stockmann, C.; Samiee-Zafarghandy, S.; King, A.D.; Deutsch, N.; Williams, E.F.; Wilkins, D.G.; Sherwin, C.M.; van den Anker, J.N. Neonatal Maturation of Paracetamol (Acetaminophen) Glucuronidation, Sulfation, and Oxidation Based on a Parent-Metabolite Population Pharmacokinetic Model. Clin. Pharmacokinet. 2016, 55, 1395–1411. [Google Scholar] [CrossRef]
- Freed, G.L.; Clark, S.J.; Butchart, A.T.; Singer, D.C.; Davis, M.M. Parental vaccine safety concerns in 2009. Pediatrics 2010, 125, 654–659. [Google Scholar] [CrossRef] [PubMed]
- Bazzano, A.; Zeldin, A.; Schuster, E.; Barrett, C.; Lehrer, D. Vaccine-related beliefs and practices of parents of children with autism spectrum disorders. American journal on intellectual and developmental disabilities 2012, 117, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Thomson, M.A.; Harvey, P.; et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998, 351, 637–641. [Google Scholar] [CrossRef]
- Schultz, S. Understanding Autism: My Quest for Nathan; Schultz Publishing LLC: 2013; pp. 92.
- Aguiar, A.G.; Mainegra, F.D.; García, R.O.; Hernandez, F.Y. Diagnosis in children with autism spectrum disorders in their development in textual comprehension. Rev Medical Sciences 2016, 20, 729–737. [Google Scholar]
- Kosteva, D. A Peek at Pharmacy Practice in Cuba. : Pharmacy Times; 2016. Availabe online: https://www.pharmacytimes.com/view/a-peek-at-pharmacy-practice-in-cuba.
- Yeldham, C. Going to Cuba? Here’s What Else To Pack. : STARTUP CUBA.TV; 2021. Availabe online: https://startupcuba.tv/2021/11/10/going-to-cuba-heres-what-else-to-pack/. (accessed on 18 December 2024).
- Sainsbury, B. 20 things to know before visiting Cuba: Lonely Planet; 2024. Availabe online: https://www.lonelyplanet.com/articles/things-to-know-before-traveling-to-cuba. (accessed on 18 December 2024).
- Preparing for Cuba: The Ultimate Packing List For Health & Safety: Simply Cuba Tours; 2023. Availabe online: https://simplycubatours.com/preparing-for-cuba-the-ultimate-packing-list-for-health-safety/. (accessed on 18 December 2024).
- How to Support Local Cubans When You Travel to Cuba: Locally Sourced Cuba Tours. Availabe online: https://locallysourcedcuba.com/how-to-support-locals-in-cuba/. (accessed on 18 December 2024).
- Maher, B. Personal genomes: The case of the missing heritability. Nature 2008, 456, 18–21. [Google Scholar] [CrossRef]
- Roberts, A.L.; Lyall, K.; Rich-Edwards, J.W.; Ascherio, A.; Weisskopf, M.G. Maternal exposure to childhood abuse is associated with elevated risk of autism. JAMA psychiatry 2013, 70, 508–515. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





