Submitted:
04 February 2025
Posted:
05 February 2025
Read the latest preprint version here
Abstract
Background. Shift workers are at increased risk for insomnia or shift work disorder. The standard treatment (cognitive behavioral therapy for insomnia) is challenging for this group. Although there are new promising approaches, they are still considered inadequate. Aims and objectives. For the present study, a customized treatment was developed in which interventions on regularity were replaced by methods to treat anxiety or depression, for example. This approach also aims to shift the focus away from disturbed sleep. Methods. Linear mixed models were used (RCT, completer analysis) to compare two active conditions (standard vs. tailored therapy) at three measurement points (pre-, post-treatment, 3-month follow-up). Primary outcomes are sleep quality, insomnia severity, sleep onset latency, and total sleep time. Secondary outcomes are anxiety, depression, tension, concern, emotional instability. Non-inferiority or equivalence tests were also performed. Results. The newly developed treatment is equivalent to standard care. Both resulted in significant and stable improvements in all variables. Thus, only the main effect across measurement points is significant, not the condition or the interaction. Outlook. Future studies should consider attrition and compliance. The treatment should be revised based on these results. The approach of improving sleep with implicit interventions should be pursued further, as it seems well suited to shift workers.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Method and Design
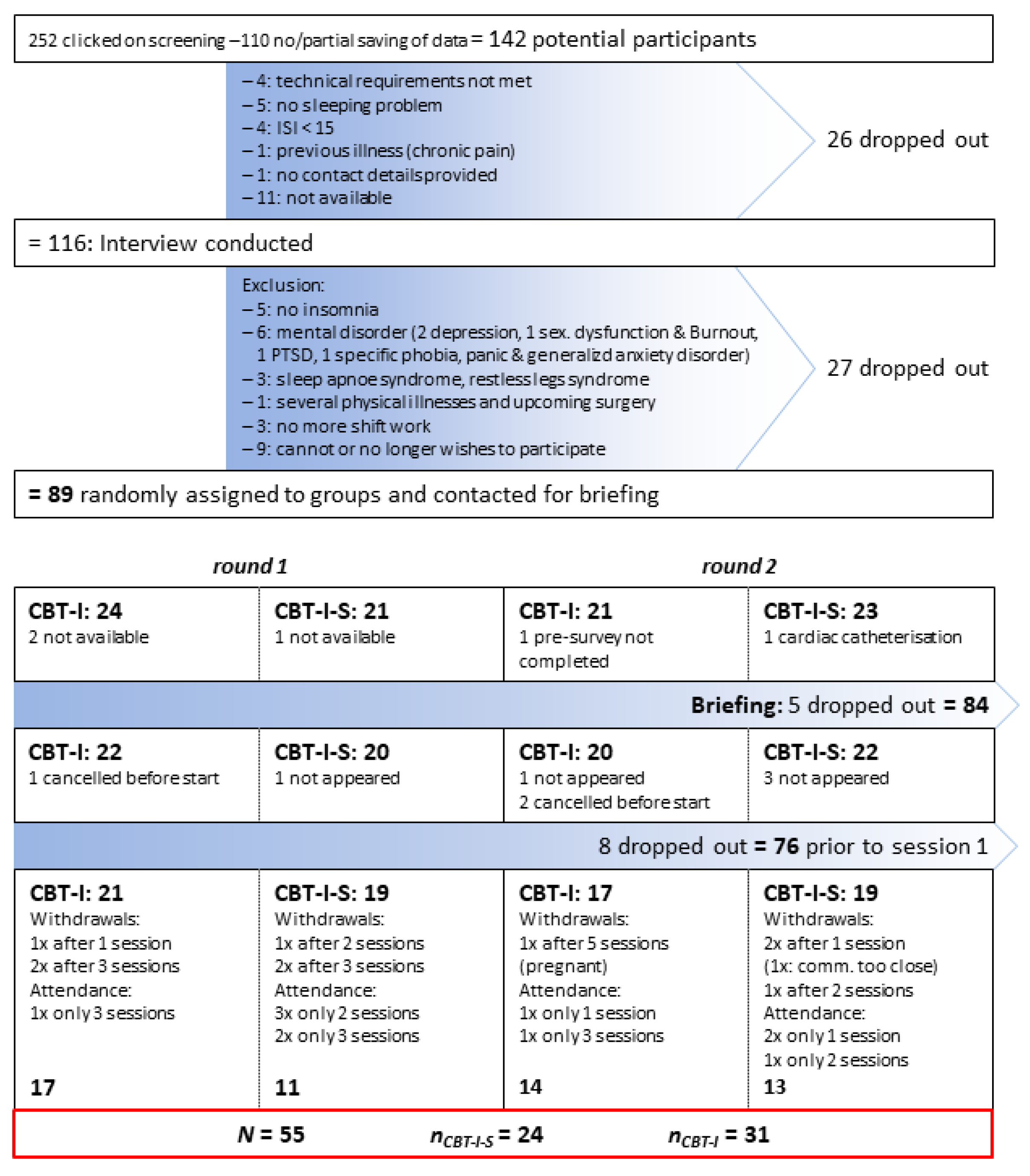
2.2. Sampling: Criteria, Procedure and Participants
2.3. Setting and Conditions of Implementation
2.4. Data Collection
| Content/Endpoint variable | T0: Screening | Interview | T1: Pre | T2: Post | T3: Follow-up | Instrument / reference |
|---|---|---|---|---|---|---|
| Screening and interview: in-/exclusion criteria | ||||||
| Age, sufficient German language skills, technical requirements, previous illnesses, insomnia (since ≥ 3 months, ≥ 3x/week; ISI ≥15), weekly working hours ≥ 30, shift work, contact details |
x | In-house developed items; ISI (Insomnia Severity Index), [17] |
||||
| Screening for mental disorders | x | Mini-DIPS (Diagnostisches Interview psychischer Störungen) [23] | ||||
| Insomnia or SWD, no other sleep disorder like Restless-Legs Syndrome, Sleep-Apnoe Syndrome | x | SIS-D-5: in-house development based on SIS-III-R [24]; DSM-5 [25]; SCID-5-CV [26]. SS-Q (Shift-specific questions) [4] |
||||
| Attitude towards shift work | x | Own item: “Do you like working shifts? Yes, I don’t mind / No, but I have to“ |
||||
| Chronotype | x | rCSM (reduced Composite Scale of Morningness) [27] | ||||
| Demographics | ||||||
| Age, gender, federal state, marital status, years of shift work, profession, shift system | x | In-house developed items |
||||
| Sleep variables | ||||||
| Sleep quality (PSQI total) „subjective sleep quality“ (SSQ, comp. 1) SOL: sleep-onset latency (item 2) TST: total sleep time (item 4) sleep efficiency (comp. 4) |
x | x | x | PSQI (Pittsburgh Sleep Quality Index) [28] | ||
| ISI: Insomnia Severity | x ≥15 |
x | x | x | ISI (Insomnia Severity Index) [17] | |
| DS: Daytime sleepiness | x | x | x | ESS (Epworth Sleepiness Scale) [29] | ||
| MZS: Dysfunctional beliefs about sleep | x | x | x | MZS (Meinungen zum Schlaf Fragebogen) [30] | ||
| Importance of sleep | x | x | x | Own item: „How important is your sleep to you?“ 1: It's not important to me, I don't think about my sleep. 2: I only think about my sleep occasionally. 3: Sleep has a normal significance for me, as for most people. 4: I think about my sleep more often than others. 5: I structure my life in a way that ensures my sleep is not compromised. |
||
| Cognitive and somatic arousal before sleep | x | x | x | PSAS (Pre-Sleep Arousal Scale) [31] | ||
| SHI: Sleep hygiene | x | x | x | SHI (Sleep Hygiene Index) [32], own translation | ||
| Psychological and personality factors | ||||||
| Anxiety, Depression, mental well-being | x | x | x | HADS-D (Hospital Anxiety and Depression Scale) [33] | ||
| Emotional stability (C), tension (Q4), concern (O) | x | x | x | 16 PF-R (16 Personality Factor Test, revised version), [34] | ||
| Feedback on therapy: - Categorical item 1-5 - Option for open feedback |
x | Please rate how helpful the training was for you overall: 1 - The training did not help me at all 2 - 3 - Somewhat helpful. Sleep and well-being have improved, but there are still complaints. 4- 5 - Very helpful! I sleep much better and feel better overall |
||||
2.5. Treatment Manuals
2.5.1. CBT-I: Standard Manual (Treatment-as-Usual)
| Sessions | Contents | Quoted / based on / adapted from …: |
|---|---|---|
| After pre-survey | Sleep diary (to keep until the last session) | [36] |
| 1. | Introduction to the programme, psycho education, implementation of relaxation method |
[37] (pp. 49–52, 75–78, 95–96); [2,38] |
| 2. | Introduction to sleep restriction, calculation of the first sleep window |
[36]; [39] (pp. 87–97) |
| 3. | Deepen sleep restriction, repeat relaxation | [39] (pp. 101–103); [2] |
| 4. | Stimulus control, adaptation of the sleep window, repeat relaxation |
[2] (pp. 22–25) |
| 5. | Sleep hygiene, sleep hygiene check; adaptation of the sleep window, repeat relaxation |
[37] (pp. 135–141); [2] |
| 6. | Cognitive restructuring of dysfunktional thoughts about sleep |
[37] (pp. 174–177) |
| 7. | Sharing experiences, reviewing sleep diaries, relapse prevention, goodbye |
[40] (pp. 189–190) |
2.5.2. CBT-I-S: Shift-Specific Manual (Experimental Condition)
| Sessions | contents | Partly in-house development, partly quoted / based on / adapted from …: |
|---|---|---|
| After pre-survey | Reading material: Psychoeducation on healthy sleep, insomnia, and treatment options | [19,38,39,40,41,42,43,44] |
| 1. | Introduction to therapy Discussion of the reading material Derivation of the therapeutic rationale Effects of attitudes towards shift work |
[15,19,38,45,46] |
| 2. | Presentation and discussion of the concept of „shift work tolerance“; Current recommendations for shift workers; positive activities (e.g., social, family, etc.); daily structure for each shift (early, late, night shift): recognize opportunities ‘despite shift work’; find an individual relaxation method |
[2,4,6,47,48,49] |
| 3. | Central methodologies are employed: Systematic problem solving, acceptance, resource orientation. |
[50] |
| 4. | (Depressive) rumination: Gratitude-/Happiness-Diary; grumbling/worrying stop; relaxation picture |
[50,51,52] |
| 5. | Anxiety / concern: decatastrophising, reality check |
[53] |
| 6. | Mood: positive activities, success spoilers, ABC-scheme, cognitive restructuring of dysfunctional (depressive) thoughts |
[49,54] |
| 7. | Sharing experiences, emergency kit, relapse prevention, feedback and goodbye | [40] |
2.6. Statistical Analyses
3. Results
3.1. Sample
3.2. Power
3.3. A priori Group Differences
3.4. Waiting List Control Group
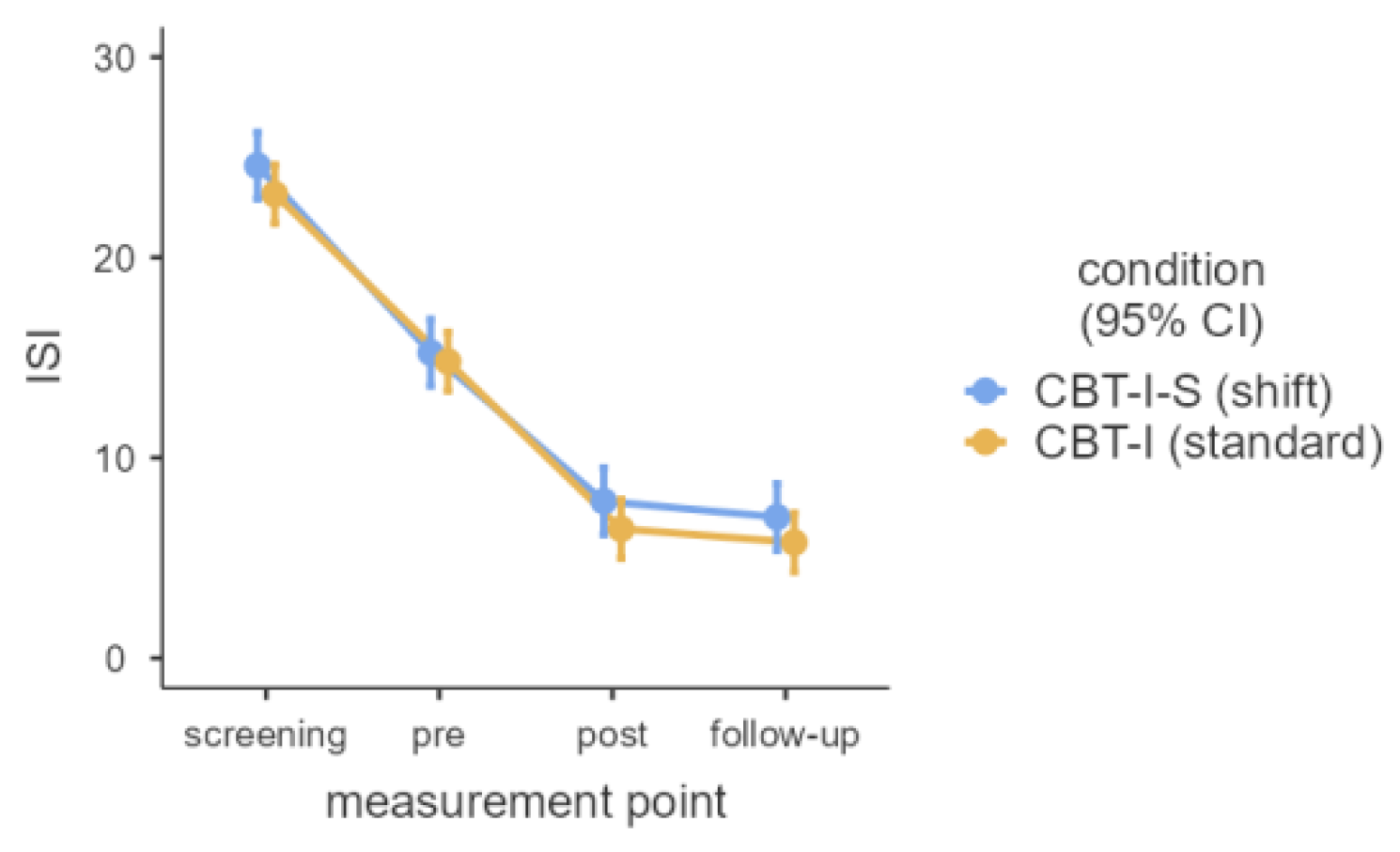
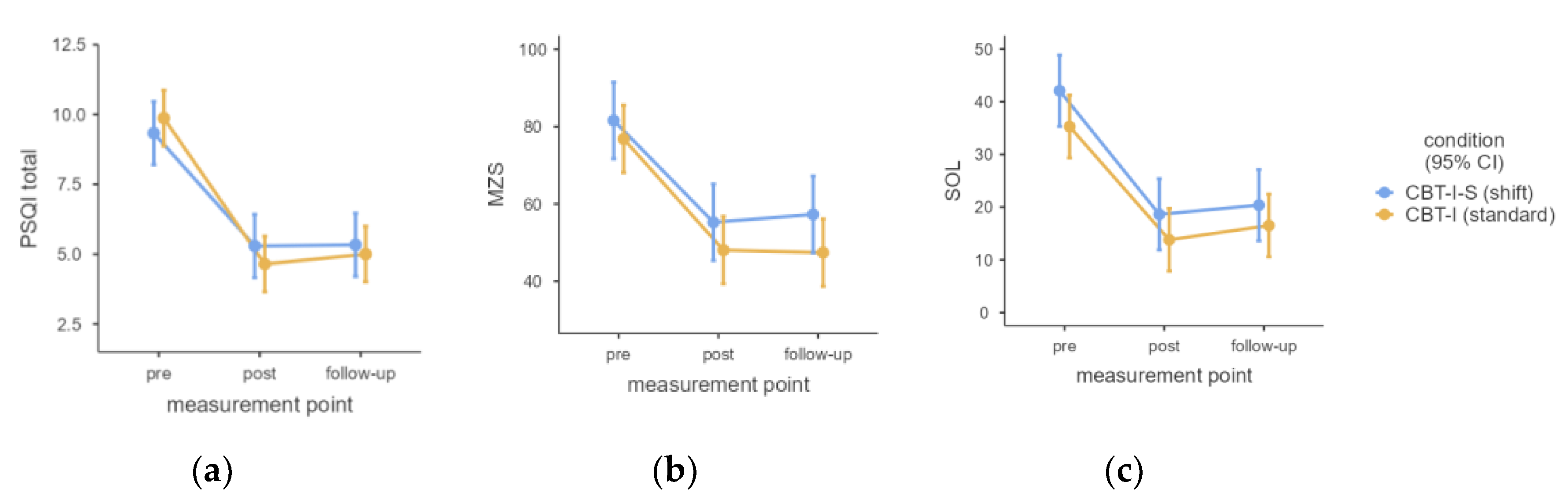
3.5. Linear Mixed Models
| Variable | Measurement point | Condition | Measurement point * Condition | ||||||
| F(2, 106) | p | η2partial | F(1, 53) | p | η2partial | F(2, 106) | p | η2partial | |
| SSQ | 51.86 | .003 | 0.49 | 0.30 | .707 | - | 1.60 | .336 | - |
| SOL | 56.16 | .003 | 0.51 | 2.00 | .298 | 0.21 | .843 | ||
| TST | 39.04 | .003 | 0.42 | 0.18 | .742 | 1.33 | .408 | ||
| Sleep efficiency | 40.86 | .003 | 0.44 | 0.02 | .904 | 1.79 | .305 | ||
| PSQI total | 80.24 | .003 | 0.60 | 0.06 | .843 | 1.10 | .470 | ||
| Importance of sleep | 7.36 | .003 | 0.12 | 0.01 | .923 | 0.71 | .633 | ||
| MZS | 64.12 | .003 | 0.55 | 1.57 | .341 | 0.42 | .742 | ||
| ISI total (3t) | 135.02 | .003 | 0.72 | 1.18 | .414 | 0.39 | .742 | ||
| ISI total (4t) (df = 3/159 rsp. 1/53) |
399.96 | .003 | 0.88 | 1.68 | .336 | 0.32 | .843 | ||
| ESS | 25.87 | .003 | 0.33 | 0.25 | .712 | 2.54 | .174 | ||
| PSAS soma | 6.50 | .006 | 0.11 | 2.49 | .225 | 3.56 | .080 | ||
| PSAS cogn | 29.69 | .003 | 0.36 | 2.59 | .219 | 1.61 | .336 | ||
| PSAS total | 22.62 | .003 | 0.30 | 2.98 | .180 | 3.19 | .108 | ||
| SHI | 21.23 | .003 | 0.29 | 6.29 | .041 | 0.11 | 0.60 | .683 | |
| HADS-A | 20.10 | .003 | 0.28 | 0.27 | .711 | 2.55 | .174 | ||
| HADS-D | 15.91 | .003 | 0.23 | 0.59 | .592 | 3.00 | .125 | ||
| HADS total | 26.25 | .003 | 0.33 | 0.50 | .633 | 4.03 | .055 | ||
| 16-PF: C emo. stab. | 7.29 | .003 | 0.12 | 1.11 | .424 | 1.03 | .492 | ||
| 16-PF: Q4 tension | 5.91 | .012 | 0.10 | 0.35 | .683 | 5.42 | .017 | 0.09 | |
| 16-PF: O concern | 8.81 | .003 | 0.14 | 1.23 | .408 | 2.58 | .174 | ||
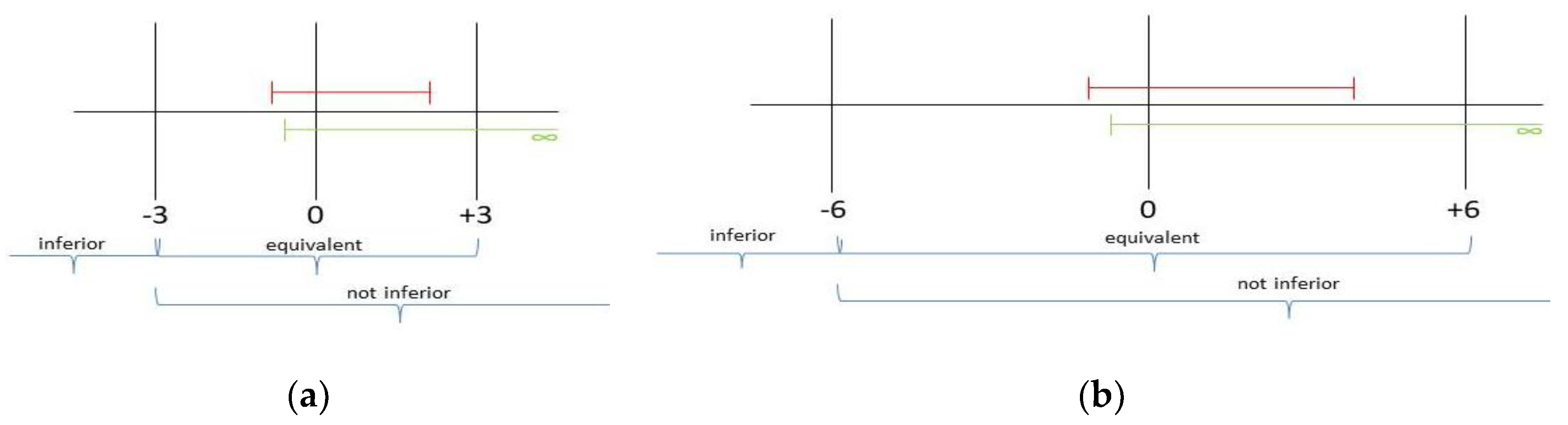
3.6. Non-Inferiority/Equivalence Tests
3.7. Remission Rates
| Screening (T0) | Pre (T1) | Post (T2) | Follow-up (T3) | ||
| ISI <15: subthreshold clinical insomnia | CBT-I-S (24) | 0 (0%) | 11 (45.83%) | 22 (91.67%) | 22 (91.67%) |
| CBT-I (31) | 0 (0%) | 15 (48.39%) | 28 (90.32%) | 30 (96.77%) | |
| ISI < 8: no clinically significant insomnia | CBT-I-S (24) | 0 (0%) | 1 (4.17%) | 12 (50.00%) | 17 (70.83%) |
| CBT-I (31) | 0 (0%) | 1 (3.23%) | 22 (70.97%) | 22 (70.97%) | |
| Difference ≥ 6 T0-T1 |
CBT-I-S (24) | 21 (87.50%) | |||
| CBT-I (31) | 26 (83.87%) | ||||
| Difference ≥ 6 T1-T2 |
CBT-I-S (24) | 17 (70.83%) | |||
| CBT-I (31) | 25 (80.65%) | ||||
| Difference ≥ 6 T2-T3 |
CBT-I-S (24) | 2 (8.33%) | |||
| CBT-I (31) | 2 (6.45%) | ||||
3.8. Feedbacks
3.9. Dropout Rates
4. Discussion
4.1. Limitations
4.2. Strengths
5. Conclusions
5.1. Outlook
Supplementary Materials
Abbreviations
| SWD | Shift work disorder |
| CBT-I | Cognitive behavioral therapy for insomnia |
| CBT-I-S | Cognitive behavioral therapy for insomnia in shift workers |
| TST | Total sleep time |
| SOL | Sleep onset latency |
| SSQ | Subjective sleep quality |
| DS | Daytime sleepiness |
| ISI | Insomnia severity index |
| PSQI | Pittsburgh sleep quality index |
| ESS | Epworth sleepiness scale |
| MZS | Meinungen-zum-Schlaf-Fragebogen |
| PSAS | Pre-sleep arousal scale |
| SHI | Sleep hygiene index |
| HADS-D | Hospital anxiety and depression scale |
| 16 PF-R | 16-Persönlichkeits-Faktoren-Test, revidierte Fassung |
| MCID | Minimal clinically important difference |
References
- Grünberger, T.; Höhn, C.; Schabus, M.; Laireiter, A.-R. Insomnia in Shift Workers: Which trait and state characteristics could serve as foundation for developing an innovative therapeutic approach? Preprints 2024. [Google Scholar] [CrossRef]
- Espie, C.A. Standard CBT-I protocol for the treatment of insomnia disorder. In Cognitive-behavioural therapy für insomnia (CBT-I) across the life span. Guidelines and clinical protocols for health professionals; Baglioni., C., Espie, C.A., Riemann, D., Eds.; John Wiley & Sons Ltd: Oxford, UK, 2022; pp. 19–41. [Google Scholar]
- Tout, A.F.; Tang, N.K.Y.; Sletten, T.L.; Toro, C.T.; Kershaw, C.; Meyer., C.; Rajaratnam, S.M.W.; Moukhtarian, T.R. Current sleep interventions for shift workers: a mini review to shape a new preventative, multicomponent sleep management programme. In Front Sleep; 2024; Volume 3. [Google Scholar] [CrossRef]
- Järnefelt, H.; Spiegelhalder, K. CBT-I Protocols for Shift Workers and Health Operators. In Cognitive-behavioural therapy für insomnia (CBT-I) across the life span. Guidelines and clinical protocols for health professionals; Baglioni., C., Espie, C.A., Riemann, D., Eds.; John Wiley & Sons Ltd: Oxford, UK, 2022; pp. 126–132. [Google Scholar]
- Kalkanis, A.; Demolder, S.; Papadopoulos, D.; Testelmans, D.; Buyse, B. Recovery from shift work. Front Neurol 2023, 14, 1270043. [Google Scholar] [CrossRef]
- Shriane, A.E.; Rigney, G.; Ferguson, S.A.; Bin, Y.S.; Vincent, G.E. Healthy sleep practices for shift workers: consensus sleep hygiene guidelines using a Delphi methodology. Sleep 2023, 46, 1–14. [Google Scholar] [CrossRef]
- Ell, J.; Brückner, H.A.; Johann, A.F.; Steinmetz, L.; Güth, L.J.; Feige, B.; Järnefelt, H.; Vallières, A.; Frase, L.; Domschke, K.; Riemann, D.; Lehr, D.; Spiegelhalder, K. Digital cognitive behavioural therapy for insomnia reduces insomnia in nurses suffering from shift work disorder: A randomised-controlled pilot trial. J. Sleep Res. 2024; 33, e14193. [Google Scholar] [CrossRef]
- Reynolds, A.C.; Sweetman, A.; Crowther, M.E.; Paterson, J.L.; Scott, H.; Lechat, B.; Wanstall, S.E.; Brown, B.W.; Lovato, N.; Adams, R.J.; Eastwood, P.R. Is cognitive behavioral therapy for insomnia (CBTi) efficacious for treating insomnia symptoms in shift workers? A systematic review and meta-analysis. Sleep Med. Rev. 2023, 67. [Google Scholar] [CrossRef] [PubMed]
- Järnefelt, H.; Lagerstedt, R.; Kajaste, S.; Sallinen, M.; Savolainen, A.; Hublin, C. Cognitive behavioral therapy for shift workers with chronic insomnia. Sleep med. 2012, 13, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Järnefelt, H.; Härmä, M.; Sallinen, M.; Virkkala, J.; Paajanen, T. Martimo, K.-P.; Hublin, C. Cognitive behavioural therapy interventions for insomnia among shift workers: RCT in an occupational health setting. Int. Arch. Occup. Environ. Health, 2020; 93, 535–550. [Google Scholar] [CrossRef]
- Booker, L.A.; Sletten, T.L.; Barnes, M.; Alvaro, P.; Collins, A.; Chai-Coetzer, C.L.; McMahon, M.; Lockley, S.W.; Rajaratnam, S.M.W.; Howard, M.E. The effectiveness of an individualized sleep and shift work education and coaching program to manage shift work disorder in nurses: a randomized controlled trial. J. Clin. Sleep Med. 2022, 18, 1035–1045. [Google Scholar] [CrossRef] [PubMed]
- Jang, E.H.; Hong, Y.; Kim, Y.; Lee, S.; Ahn, Y.; Jeong, K.S.; Jang, T.-W.; Lim, H.; Jung, E.; Chung, S.; Shift Work Disorder Study Group; Suh, S. The development of a sleep intervention for firefighters: The FIT-IN (Firefighter’s Therapy for Insomnia and Nightmares) Study. In Int. J. Environ. Res. Public Health; 2020; Volume 17. [Google Scholar] [CrossRef]
- Takano, Y.; Ibata, R.; Machida, N.; Ubara, A.; Okajima, I. Effect of cognitive behavioral therapy for insomnia in workers: A systematic review and meta-analysis of randomized controlled trials. Sleep Med. Rev. 2023, 71. [Google Scholar] [CrossRef]
- Bastille-Denis, E.; Lemyre, A.; Pappathomas, A.; Roy, M.; Vallières, A. Are cognitive variables that maintain insomnia also involved in shift work disorder? Sleep Health 2020, 6, 399–406. [Google Scholar] [CrossRef]
- Harvey, A.G. A cognitive model of insomnia. Behav. Res. Ther. 2002, 40, 869–893. [Google Scholar] [CrossRef]
- Vallières, A.; Pappathomas, A.; Garnier, S.B.; Mérette, C.; Carrier, J.; Paquette, T.; Bastien, C.H. Behavioural therapy for shift work disorder improves shift workers' sleep, sleepiness and mental health: A pilot randomised control trial. J. Sleep Res. 2024; 33, e14162. [Google Scholar] [CrossRef]
- Gerber, M.; Lang, C.; Lemola, S.; Colledge, F.; Kalak, N.; Holsboer-Trachsler, E.; Pühse, U.; Brand, S. Validation of the German version of the insomnia severity index in adolescents, young adults and adult workers: results from three cross-sectional studies. BMC Psychiatry 2016, 16, 1–14. [Google Scholar] [CrossRef]
- Yang, M.; Morin, C.M.; Schaefer, K.; Wallenstein, G.V. Interpreting score differences in the Insomnia Severity Index: using health-related outcomes to define the minimally important difference. Curr. Med. Res. Opin. 2009, 25, 2487–2494. [Google Scholar] [CrossRef]
- Espie, C.A.; Broomfield, N.M.; MacMahon, K.M.; Macphee, L.M.; Taylor, L.M. The attention-intention-effort pathway in the development of psychophysiologic insomnia: a theoretical review. Sleep Med. Rev. 2006, 10, 215–245. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Buchner, A.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods, 2007; 39, 175–191. [Google Scholar]
- Espie, C.A.; Kyle, S.D.; Williams, C.; Ong, J.C.; Douglas, N.J.; Hames, P.; Brown, J.S.L. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep 2012, 35, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Drake, C.L. Psychological impact of shift work. Curr. Sleep Med. Rep. 2018, 4, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Margraf, J.; Cwik, J.C. Mini-DIPS Open Access: Diagnostisches Kurzinterview bei psychischen Störungen. Forschungs- und Behandlungszentrum für psychische Gesundheit, Ruhr-Universität Bochum: Bochum, Germany, 2017. [Google Scholar] [CrossRef]
- Schramm, E.; Hohagen, F.; Graßhoff, U.; Berger, M. Strukturiertes Interview für Schlafstörungen nach DSM-III-R. Beltz Test GmbH: Weinheim, Germany, 1991. [Google Scholar]
- American Psychiatric Association (APA, 2013). Diagnostic and statistical manual of mental disorders, fifth edition, DSM-5. American Psychiatric Association: Arlington, USA, 2013.
- Beesdo-Baum, K.; Zaudig, M.; Wittchen, H.-U. (Eds.) . SCID-5-CV. Strukturiertes Klinisches Interview für DSM-5R-Störungen – Klinische Version. Deutsche Bearbeitung des Stuctured Clinical Interview for CDM-5R Disorders – Clinician Version von Michael B. First, Jane B. Williams, Rhonda S. Hogrefe: Göttingen, Germany, 2019.
- Randler, C. Psychometric properties of the German version of the Composite Scale of Morningness. Biol. Rhythm Res. 2008, 39, 151–161. [Google Scholar] [CrossRef]
- Riemann, D.; Backhaus, J. Behandlung von Schlafstörungen. Psychologie Verlags Union: Weinheim, Germany, 1996.
- Bloch, K.E.; Schoch, O.D.; Zhang, J.N.; Russi, E.W. German version of the Epworth Sleepiness Scale. Respiration 1999, 66, 440–447. [Google Scholar] [CrossRef]
- Weingartz, S.; Pillmann, F. Meinungen-zum-Schlaf-Fragebogen. Deutsche Version der DBAS-16 zur Erfassung dysfunktionaler Überzeugungen und Einstellungen zum Schlaf. Somnologie, 2009; 13, 29–36. [Google Scholar] [CrossRef]
- Gieselmann, A.; de Jong-Mayer, R.; Pietrowsky, R. Kognitive und körperliche Erregung in der Phase vor dem Einschlafen. Die deutsche Version der Pre-Sleep Arousal Scale (PSAS). Z Kl. Psych. Psychoth. 2012; 41, 73–80. [Google Scholar]
- Mastin, D.F.; Bryson, J.; Corwyn, R. Assessment of sleep hygiene using the Sleep Hygiene Index. J. Behav. Med. 2006, 29, 223–227. [Google Scholar] [CrossRef]
- Herrmann-Lingen, C.; Buss, U.; Snaith, R.P. Hospital Anxiety and Depression Scale, Deutsche Version (HADS-D) (Vol. 3). Huber: Bern, Switzerland, 2011.
- Schneewind, K.A.; Graf, J. Der 16-Persönlichkeits-Faktoren-Test, revidierte Fassung. 16 PF-R – deutsche Ausgabe des 16 PF Fifth Edition – Testmanual. Hans Huber: Bern, Switzerland, 1998.
- Grünberger, T.; Höhn, C.; Schabus, M.; Laireiter, A.-R. Efficacy study comparing a CBT-I developed for shift workers (CBT-I-S) to standard CBT-I (cognitive behavioural therapy for insomnia) on sleep onset latency, total sleep time, subjective sleep quality, and daytime sleepiness: study protocol for a parallel group randomized controlled trial with online therapy groups of seven sessions each. Trials 2024, 25, 1–10. [Google Scholar] [CrossRef]
- Scharfenstein, A.; Basler, H.-D. Schlafstörungen. Auf dem Weg zu einem besseren Schlaf. Schlaftagebuch. Vandenhoeck & Ruprecht: Göttingen, Germany, 2004. [Google Scholar]
- Binder, R.; Schöller, F.; Weeß, H.-G. Therapie-Tools Schlafstörungen. Beltz: Weinheim, Germany, 2020.
- Crönlein, T. Primäre Insomnie. Ein Gruppentherapieprogramm für den stationären Bereich. Hogrefe: Göttingen, Germany, 2013.
- Müller, T.; Paterok, B. Schlaftraining. Ein Therapiemanual zur Behandlung von Schlafstörungen, (2., überarbeitete Auflage). Hogrefe: Göttingen, Germany, 2010. [Google Scholar]
- Scharfenstein, A.; Basler, H.-D. Schlafstörungen. Auf dem Weg zu einem besseren Schlaf. Trainerhandbuch, Vandenhoeck & Ruprecht: Göttingen, Germany,, 2004. [Google Scholar]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders, third edition: (ICSD-3). American Academy of Sleep Medicine: Darien, IL, USA, 2014.
- Baglioni, C.; Espie, C.A.; Riemann, D. (Eds.) . Cognitive-behavioral therapy for insomnia (CBT-I) across the life span. Guidelines and clinical protocols for health professionals. John Wiley & Sons Ltd: Chichester, UK, 2022.
- Pollmächer, T.; Wetter, T.C.; Bassetti, C.L.A.; Högl, B.; Randerath, W.; Wiater, A. (Eds.) . Handbuch Schlafmedizin. Elsevier: München, Germany, 2020.
- Kerkhof, G.A. Shift work and sleep disorder comorbidity tend to go hand in hand. Chronobiol. Int. 2018, 35, 219–228. [Google Scholar] [CrossRef]
- Åkerstedt, T.; Sallinen, M.; Kecklund, G. Shiftworkers’ attitude to their work hours, positive or negative, and why? Int. Arch. Occup. Environ. Health 2022, 95, 1267–1277. [Google Scholar] [CrossRef]
- Axelsson, J.; Åkerstedt, T.; Kecklund, G.; Lowden, A. Tolerance to shift work—how does it relate to sleep and wakefulness? Int. Arch. Occup. Environ. Health 2004, 77, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Reinberg, A.; Ashkenazi, I. Internal desynchronization of circadian rhythms and tolerance to shift work. Chronobiol. Int. 2008, 25, 625–643. [Google Scholar] [CrossRef] [PubMed]
- Saksvik, I.B.; Bjorvatn, B.; Hetland, H.; Sandal, G.M.; Pallesen, S. Individual differences in tolerance to shift work – a systematic review. Sleep Med. Rev. 2011, 15, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Schaub, A.; Roth, E.; Goldmann, U. Kognitiv-psychoedukative Therapie zur Bewältigung von Depression. Ein Therapiemanual (2. Aufl.). Hogrefe: Göttingen, Germany, 2013.
- Teismann, T.; Hanning, S.; Brachel, R.v. , Willutzki, U. Kognitive Verhaltenstherapie depressiven Grübelns. Springer: Berlin, Germany. 2012. [Google Scholar]
- Feld, A. Rudy, J.M. (2017). Coaching der Positiven Psychologie. Manual für Coaches, [Unpublished: manual]. Paris-Lodron-Universität Salzburg, 2017. [Google Scholar]
- Spiegelhalder, K.; Backhaus, J.; Riemann, D. Schlafstörungen (2. überarbeitete Auflage). Hogrefe: Göttingen, Germany, 2011.
- Becker, E.; Margraf, J. Generalisierte Angststörung. Ein Therapieprogramm. Beltz: Weinheim, Germany, 2002.
- Pitschel-Walz, G.; Bäuml, J.; Kissling, W. Psychoedukation bei Depressionen. Manual zur Leitung von Patienten- und Angehörigengruppen. Urban & Fischer Verlag: München, Germany, 2003.
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc., Series B (Methodological) 1995, 57, 289–300. http://www.jstor.org/stable/2346101.
- Hemmerich, W. (2016). StatistikGuru: Rechner zur Adjustierung des α-Niveaus. Retrieved/: from https://statistikguru.de/rechner/adjustierung-des-alphaniveaus.html.
- Wellek, S.; Blettner, M. Klinische Studien zum Nachweis von Äquivalenz oder Nichtunterlegenheit. Teil 20 der Serie zur Bewertung wissenschaftlicher Publikationen. [Establishing equivalence or non-inferiority in clinical trials—part 20 of a series on evaluation of scientific publications]. Dtsch Arztebl Int, 2012; 109, 674–679. [Google Scholar] [CrossRef]
- Cao, S.; Xin, B.; Yu, Y.; Peng, C.; Zhu, C.; Deng, M.; Gao, X.; Chu, J.; Liu, T. Improvement of sleep quality in isolated metastatic patients with spinal cord compression after surgery. World J. Surg. Oncol. 2023, 21, 1–9. [Google Scholar] [CrossRef]
- Cohen, J. Statistical power analysis for the behavioral sciences (2nd ed.). L. Erlbaum Associates: Hillsdale, N.J.; USA, 1988.
- IBM Corp. IBM SPSS Statistics for Windows, Version 29.0.2.0. IBM Corp.: Armonk, NY, USA, 2023.
- The jamovi project. jamovi. (Version/: 2.3). Retrieved from https://www.jamovi.org.
- Vanttola, P.; Puttonen, S.; Karhula, K.; Oksanen, T.; Härmä, M. Prevalence of shift work disorder among hospital personnel: A cross-sectional study using objective working hour data. J. Sleep Res. 2020, 29, e12906. [Google Scholar] [CrossRef]
- Frank, J.D. Persuasion and healing: A comparative study of psychotherapy. John Hopkins University Press: Baltimore, MD, USA, 1961.
- Constantino, M.J.; Vîslă, A.; Coyne, A.E.; Boswell, J.F. A meta-analysis of the association between patients’ early treatment outcome expectation and their posttreatment outcomes. Psychotherapy 2018, 55, 473–485. [Google Scholar] [CrossRef]
- Pagano, R.R. (2010). Understanding statistics in the behavioral sciences, (9th ed.)., B: Thomson Wadsworth: Belmont, CA, Australia, 2010. [Google Scholar]
- Rasch, D.; &, *!!! REPLACE !!!*; Guiard, V. The robustness of parametric statistical methods. Psychol. Sci. 2004, 46, 175–208. [Google Scholar]
- Wilcox, R.R. Introduction to robust estimation and hypothesis testing (3rd ed.). Statistical modeling and decision science. Academic Press (Elsevier): Waltham, MA 02451, USA, 2012.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





