Submitted:
02 February 2025
Posted:
03 February 2025
Read the latest preprint version here
Abstract
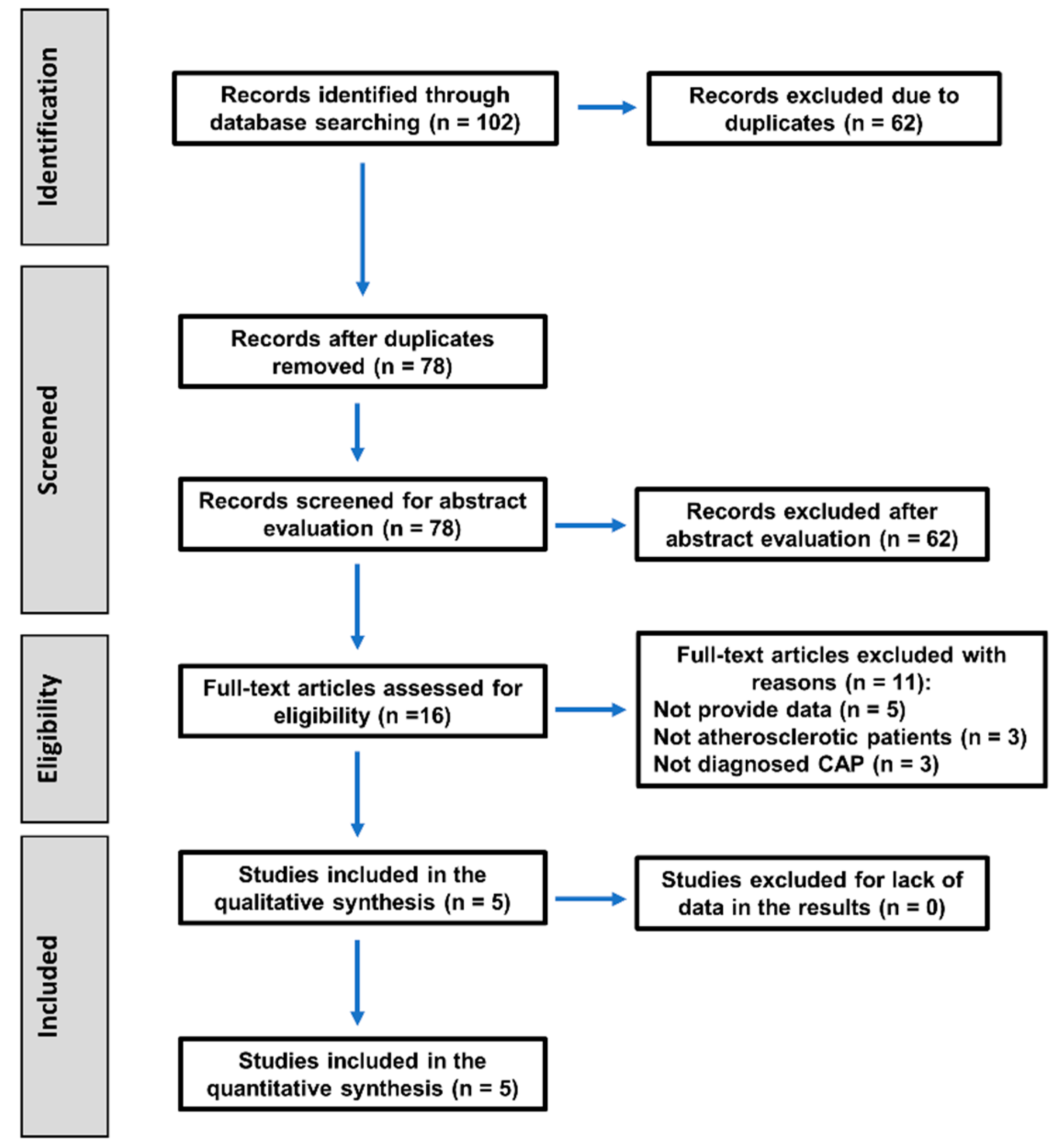
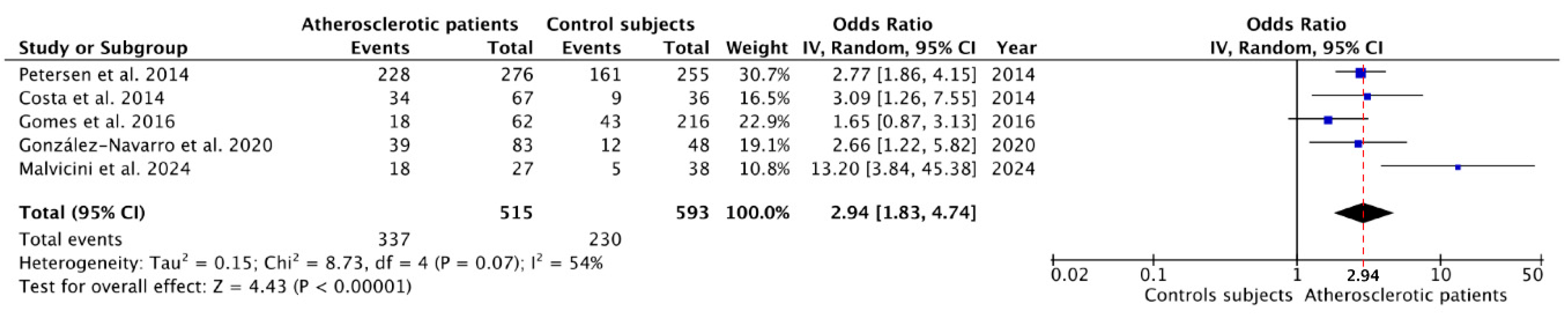
Background. Atherosclerosis is a chronic and progressive condition of the arteries, characterized by the thickening and hardening of their walls due to the formation of atherosclerotic plaques. Low-grade inflammation is implicated in the pathogeny of atherosclerosis. Chronic apical periodontitis (CAP), the chronic inflammation around the root apex of infected teeth, is associated with a low-grade inflammatory state, so a connection between atherosclerosis and CAP have been suggested. The aim of this study was to conduct a systematic review with meta-analysis to answer the following PICO question: In adult patients, does the presence or absence of atherosclerosis affect the prevalence of CAP? Methods. The PRISMA guidelines were followed to carry out this systematic review. A bibliographic search was performed in PubMed-MEDLINE, Embase, and Scielo. Inclusion criteria selected the studies presenting data on the prevalence of CAP in patients diagnosed with atherosclerosis and control patients. The statistical analysis was carried out using RevMan software software. Study characteristics and risk ratios with 95% confidence intervals (CIs) were extracted. Random-effects meta-analyses were performed. Risk of bias was assessed using the Newcastle-Ottawa scale, adapted for cross-sectional studies. To estimate variance and heterogeneity between trials, the Higgins I2 test was used. The quality of the evidence was evaluated using GRADE. Results. The search strategy recovered 102 articles, and only five met the inclusion criteria. Meta-analysis showed and overall OR = 2.94 (95% CI = 1.83 – 4.74; p < 0.01) for the prevalence of CAP among patients with atherosclerosis. The overall risk of bias was moderate. The quality of the evidence showed a low level of certainty. Conclusions. Patients with atherosclerosis are almost three times more likely to have CAP. This finding supports the hypothesis that chronic inflammatory processes in the oral cavity could significantly impact cardiovascular health, emphasizing the importance of an integrated approach to oral and systemic health care. This result should be translated to daily clinical practice: the healthcare community should be aware of this association and suspect atherosclerotic pathology in patients who show a high prevalence of CAP. Likewise, patients with atherosclerosis should be monitored in the dental clinic for CAP.
Keywords:
1. Introduction
2. Materials and Methods
2.1. Review Question
2.2. Eligibility Criteria
2.3. Search Strategy and Information Sources
2.4. Data Extraction
2.5. Data Synthesis and Analysis
2.6. Risk of Bias Assessment
2.7. Grading Recommendations Assessment, Development and Evaluation
3. Results
3.1. Characteristics of the Included Studies
3.2. Meta-Analysis of the Prevalence of Chronic Apical Periodontitis
3.3. Risk of Bias Assessment
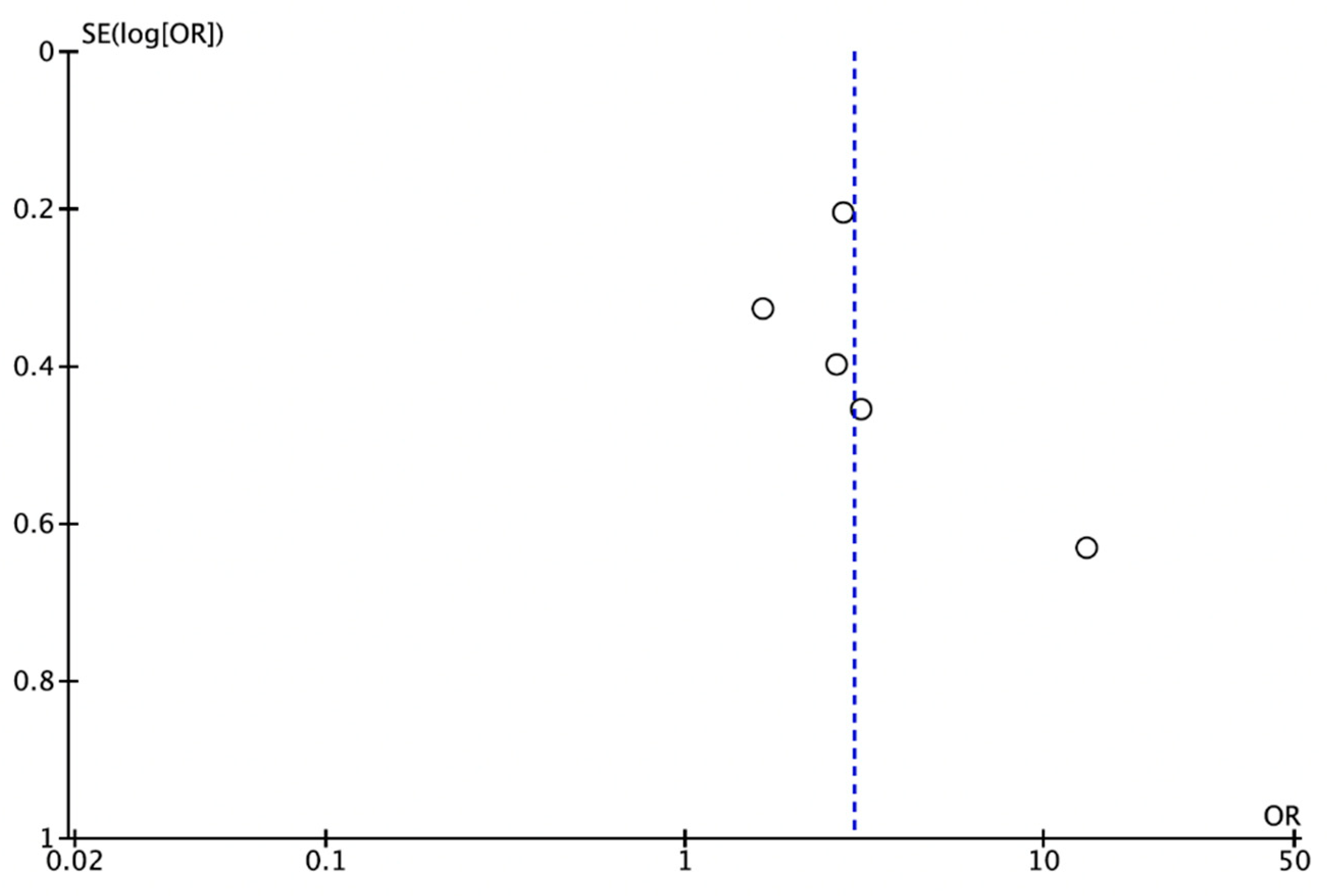
3.4. Publication Bias
3.5. GRADE Evaluation: Level of Certainty
- Detailed in Table 4: Risk of bias summary (moderate).
- I2 = 54% (p=0.07).
- 95% CI out of 0.75-1.25
4. Discussion
4.1. Methodological Differences and Heterogeneity
4.2. Pathophysiological Implications
4.3. Clinical Implications
4.4. Strengths and Limitations of the Study
4.5. Future Directions
5. Conclusions
Funding
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CAP | Chronic apical periodontitis |
| CT CI |
Confidence interval Computed tomography |
| OR | Odds ratio |
References
- Siqueira, J.F.; Rôças, I.N. The microbiota of acute apical abscesses. J. Dent. Res. 2009, 88, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Tibúrcio-Machado, C.S.; Michelon, C.; Zanatta, F.B.; Gomes, M.S.; Marin, J.A.; Bier, C.A. The global prevalence of apical periodontitis: a systematic review and meta-analysis. Int. Endod. J. 2021, 54, 712–735. [Google Scholar] [CrossRef] [PubMed]
- Orstavik, D.; Kerekes, K.; Eriksen, H.M.; Ørstavik, D.; Kerekes, K.; Eriksen, H.M. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Dent. Traumatol. 1986, 2, 20–34. [Google Scholar] [CrossRef]
- Libby, P. The changing landscape of atherosclerosis. Nature 2021, 592, 524–533. [Google Scholar] [CrossRef]
- Mushenkova, N. V.; Summerhill, V.I.; Zhang, D.; Romanenko, E.B.; Grechko, A. V.; Orekhov, A.N. Current Advances in the Diagnostic Imaging of Atherosclerosis: Insights into the Pathophysiology of Vulnerable Plaque. Int. J. Mol. Sci. 2020, 21. [Google Scholar] [CrossRef]
- Gusev, E.; Sarapultsev, A. Atherosclerosis and Inflammation: Insights from the Theory of General Pathological Processes. Int. J. Mol. Sci. 2023, 24. [Google Scholar] [CrossRef]
- Moutsopoulos, N.M.; Madianos, P.N. Low-grade inflammation in chronic infectious diseases: paradigm of periodontal infections. Ann. N. Y. Acad. Sci. 2006, 1088, 251–264. [Google Scholar] [CrossRef]
- Cotti, E.; Dessì, C.; Piras, A.; Mercuro, G. Can a chronic dental infection be considered a cause of cardiovascular disease? A review of the literature. Int. J. Cardiol. 2011, 148, 4–10. [Google Scholar] [CrossRef]
- Papi, P.; Pranno, N.; Di Murro, B.; Pompa, G.; Polimeni, A.; Letizia, C.; Petramala, L.; Concistrè, A.; Muñoz Aguilera, E.; Orlandi, M.; et al. Association between subclinical atherosclerosis and oral inflammation: A cross-sectional study. J. Periodontol. 2023, 94, 477–486. [Google Scholar] [CrossRef]
- Doughan, M.; Chehab, O.; de Vasconcellos, H.D.; Zeitoun, R.; Varadarajan, V.; Doughan, B.; Wu, C.O.; Blaha, M.J.; Bluemke, D.A.; Lima, J.A.C. Periodontal Disease Associated With Interstitial Myocardial Fibrosis: The Multiethnic Study of Atherosclerosis. J. Am. Heart Assoc. 2023, 12. [Google Scholar] [CrossRef]
- Chauhan, N.; Mittal, S.; Tewari, S.; Sen, J.; Laller, K. Association of Apical Periodontitis with Cardiovascular Disease via Noninvasive Assessment of Endothelial Function and Subclinical Atherosclerosis. J. Endod. 2019, 45, 681–690. [Google Scholar] [CrossRef] [PubMed]
- Cotti, E.; Dess, C.; Piras, A.; Flore, G.; Deidda, M.; Madeddu, C.; Zedda, A.; Longu, G.; Mercuro, G. Association of endodontic infection with detection of an initial lesion to the cardiovascular system. J. Endod. 2011, 37, 1624–1629. [Google Scholar] [CrossRef] [PubMed]
- Gomes, M.S.; Hugo, F.N.; Hilgert, J.B.; Sant’Ana Filho, M.; Padilha, D.M.P.; Simonsick, E.M.; Ferrucci, L.; Reynolds, M.A. Apical periodontitis and incident cardiovascular events in the Baltimore Longitudinal Study of Ageing. Int. Endod. J. 2016, 49, 334–342. [Google Scholar] [CrossRef]
- Cabanillas-Balsera, D.; Areal-Quecuty, V.; Cantiga-Silva, C.; de Cardoso, C.B.M.; Cintra, L.T.A.; Martín-González, J.; Segura-Egea, J.J. Prevalence of apical periodontitis and non-retention of root-filled teeth in hypertensive patients: Systematic review and meta-analysis. Int. Endod. J. 2023, 256–269. [Google Scholar] [CrossRef]
- Leão, T.S.S.; Tomasi, G.H.; Conzatti, L.P.; Marrone, L.C.P.; Reynolds, M.A.; Gomes, M.S. Oral Inflammatory Burden and Carotid Atherosclerosis Among Stroke Patients. J. Endod. 2022, 48, 597–605. [Google Scholar] [CrossRef]
- Conti, L.C.; Segura-Egea, J.J.; Cardoso, C.B.M.; Benetti, F.; Azuma, M.M.; Oliveira, P.H.C.; Bomfim, S.R.M.; Cintra, L.T.A. Relationship between apical periodontitis and atherosclerosis in rats: lipid profile and histological study. Int. Endod. J. 2020. [CrossRef]
- Gan, G.; Lu, B.; Zhang, R.; Luo, Y.; Chen, S.; Lei, H.; Li, Y.; Cai, Z.; Huang, X. Chronic apical periodontitis exacerbates atherosclerosis in apolipoprotein E-deficient mice and leads to changes in the diversity of gut microbiota. Int. Endod. J. 2021, 1–12. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Estarli, M.; Barrera, E.S.A.; et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev. Esp. Nutr. Humana y Diet. 2016, 20, 148–160. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 1–11. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Herzog, R.; Álvarez-Pasquin, M.J.; Díaz, C.; Del Barrio, J.L.; Estrada, J.M.; Gil, Á. Are healthcare workers intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- León-López, M.; Cabanillas-Balsera, D.; Martín-González, J.; Montero-Miralles, P.; Saúco-Márquez, J.J.; Segura-Egea, J.J. Prevalence of root canal treatment worldwide: A systematic review and meta-analysis. Int. Endod. J. 2022, 55, 1105–1127. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.; Kunz, R.; Brozek, J.; Alonso-Coello, P.; Montori, V.; Akl, E.A.; Djulbegovic, B.; Falck-Ytter, Y.; et al. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). J. Clin. Epidemiol. 2011, 64, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Hultcrantz, M.; Rind, D.; Akl, E.A.; Treweek, S.; Mustafa, R.A.; Iorio, A.; Alper, B.S.; Meerpohl, J.J.; Murad, M.H.; Ansari, M.T.; et al. The GRADE Working Group clarifies the construct of certainty of evidence. J. Clin. Epidemiol. 2017, 87, 4–13. [Google Scholar] [CrossRef]
- Friedlander, A.H.; Sung, E.C.; Chung, E.M.; Garrett, N.R. Radiographic quantification of chronic dental infection and its relationship to the atherosclerotic process in the carotid arteries. Oral Surgery, Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 109, 615–621. [Google Scholar] [CrossRef]
- Glodny, B.; Nasseri, P.; Crismani, A.; Schoenherr, E.; Luger, A.; Bertl, K.; Petersen, J. The occurrence of dental caries is associated with atherosclerosis. Clinics 2013, 68, 946–953. [Google Scholar] [CrossRef]
- Liljestrand, J.M.; Mäntylä, P.; Paju, S.; Buhlin, K.; Kopra, K.A.E.; Persson, G.R.; Hernandez, M.; Nieminen, M.S.; Sinisalo, J.; Tjäderhane, L.; et al. Association of Endodontic Lesions with Coronary Artery Disease. J. Dent. Res. 2016, 95, 1358–1365. [Google Scholar] [CrossRef]
- Willershausen, B.; Kasaj, A.; Willershausen, I.; Zahorka, D.; Briseño, B.; Blettner, M.; Genth-Zotz, S.; Münzel, T. Association between Chronic Dental Infection and Acute Myocardial Infarction. J. Endod. 2009, 35, 626–630. [Google Scholar] [CrossRef]
- Pasqualini, D.; Bergandi, L.; Palumbo, L.; Borraccino, A.; Dambra, V.; Alovisi, M.; Migliaretti, G.; Ferraro, G.; Ghigo, D.; Bergerone, S.; et al. Association among oral health, apical periodontitis, CD14 polymorphisms, and coronary heart disease in middle-aged adults. J. Endod. 2012, 38, 1570–1577. [Google Scholar] [CrossRef]
- Frisk, F.; Hakeberg, M.; Ahlqwist, M.; Bengtsson, C. Endodontic variables and coronary heart disease. Acta Odontol. Scand. 2003, 61, 257–262. [Google Scholar] [CrossRef]
- Jansson, L.; Lavstedt, S.; Frithiof, L.; Theobald, H. Relationship between oral health and mortality in cardiovascular diseases. J. Clin. Periodontol. 2001, 28, 762–8. [Google Scholar] [CrossRef] [PubMed]
- Cowan, L.T.; Lakshminarayan, K.; Lutsey, P.L.; Beck, J.; Offenbacher, S.; Pankow, J.S. Endodontic therapy and incident cardiovascular disease: The Atherosclerosis Risk in Communities (ARIC) study. J. Public Health Dent. 2020, 80, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; He, M.; Yin, T.; Zheng, Z.; Fang, C.; Peng, S. Association of severely damaged endodontically infected tooth with carotid plaque and abnormal carotid intima-media thickness: a retrospective analysis. Clin. Oral Investig. 2023, 27, 4677–4686. [Google Scholar] [CrossRef] [PubMed]
- Petersen, J.; Glaßl, E.-M.M.; Nasseri, P.; Crismani, A.; Luger, A.K.; Schoenherr, E.; Bertl, K.; Glodny, B. The association of chronic apical periodontitis and endodontic therapy with atherosclerosis. Clin. Oral Investig. 2014, 18, 1813–1823. [Google Scholar] [CrossRef] [PubMed]
- Costa, T.H.R.; Neto, J.A.D.F.; De Oliveira, A.E.F.; Maia, M.D.F.L.E.; de Almeida, A.L.; de Figueiredo Neto, J.A.; De Oliveira, A.E.F.; Lopes e Maia, M. de F; de Almeida, A.L. Association between chronic apical periodontitis and coronary artery disease. J. Endod. 2014, 40, 164–7. [Google Scholar] [CrossRef]
- González-Navarro, B.; Segura-Egea, J.J.; Estrugo-Devesa, A.; Pintó-Sala, X.; Jane-Salas, E.; Jiménez-Sánchez, M.C.; Cabanillas-Balsera, D.; López-López, J. Relationship between apical periodontitis and metabolic syndrome and cardiovascular events: A cross-sectional study. J. Clin. Med. 2020, 9, 1–13. [Google Scholar] [CrossRef]
- Malvicini, G.; Marruganti, C.; Leil, M.A.; Martignoni, M.; Pasqui, E.; de Donato, G.; Grandini, S.; Gaeta, C. Association between apical periodontitis and secondary outcomes of atherosclerotic cardiovascular disease: A case–control study. Int. Endod. J. 2024, 57, 281–296. [Google Scholar] [CrossRef]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalgh, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H. The 2011 Oxford CEBM Levels of Evidence: Introductory Document. Oxford Cent. Evidence-Based Med. http//www.cebm.net/index.aspx?o=5653 2011, 1–3.
- Ríos-Santos, J. V.; Ridao-Sacie, C.; Bullón, P.; Fernández-Palacín, A.; Segura-Egea, J.J. Assessment of periapical status: A comparative study using film-based periapical radiographs and digital panoramic images. Med. Oral Patol. Oral Cir. Bucal 2010, 15. [Google Scholar] [CrossRef]
- Lo Giudice, R.; Nicita, F.; Puleio, F.; Alibrandi, A.; Cervino, G.; Lizio, A.S.; Pantaleo, G. Accuracy of Periapical Radiography and CBCT in Endodontic Evaluation. Int. J. Dent. 2018, 2018, 1–7. [Google Scholar] [CrossRef]
- Patel, S.; Durack, C.; Abella, F.; Roig, M.; Shemesh, H.; Lambrechts, P.; Lemberg, K. European Society of Endodontology position statement: The use of CBCT in Endodontics. Int. Endod. J. 2014, 47, 502–504. [Google Scholar] [CrossRef]
- HILL, A.B. THE ENVIRONMENT AND DISEASE: ASSOCIATION OR CAUSATION? Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Segura-Egea, J.J.; Martín-González, J.; Castellanos-Cosano, L. Endodontic medicine: connections between apical periodontitis and systemic diseases. Int. Endod. J. 2015, 48, 933–951. [Google Scholar] [CrossRef] [PubMed]
- Cotti, E.; Zedda, A.; Deidda, M.; Piras, A.; Flore, G.; Ideo, F.; Madeddu, C.; Pau, V.M.; Mercuro, G. Endodontic Infection and Endothelial Dysfunction Are Associated with Different Mechanisms in Men and Women. J. Endod. 2015, 41, 594–600. [Google Scholar] [CrossRef]
- Soysal, P.; Arik, F.; Smith, L.; Jackson, S.E.; Isik, A.T. Inflammation, Frailty and Cardiovascular Disease. Adv. Exp. Med. Biol. 2020, 1216, 55–64. [Google Scholar] [CrossRef]
- Georgiou, A.C.; Twisk, J.W.R.; Crielaard, W.; Ouwerling, P.; Schoneveld, A.H.; van der Waal, S.V. The influence of apical periodontitis on circulatory inflammatory mediators in peripheral blood: A prospective case-control study. Int. Endod. J. 2023, 56, 130–145. [Google Scholar] [CrossRef]
- Aarabi, G.; Heydecke, G.; Seedorf, U. Roles of Oral Infections in the Pathomechanism of Atherosclerosis. Int. J. Mol. Sci. 2018, 19. [Google Scholar] [CrossRef]
- Georgiou, A.C.; Crielaard, W.; Armenis, I.; de Vries, R.; van der Waal, S. V. Apical Periodontitis Is Associated with Elevated Concentrations of Inflammatory Mediators in Peripheral Blood: A Systematic Review and Meta-analysis. J. Endod. 2019, 45, 1279–1295e3. [Google Scholar] [CrossRef]
- Segura-Egea, J.J.; Cabanillas-Balsera, D.; Martín-González, J.; Cintra, L.T.A. Impact of systemic health on treatment outcomes in endodontics. Int. Endod. J. 2023, 56 Suppl 2, 219–235. [Google Scholar] [CrossRef]
- Sirin, D.A.; Ozcelik, F.; Uzun, C.; Ersahan, S.; Yesilbas, S. Association between C-reactive protein, neutrophil to lymphocyte ratio and the burden of apical periodontitis: a case-control study. Acta Odontol. Scand. 2019, 77, 142–149. [Google Scholar] [CrossRef]
- Hajishengallis, G.; Chavakis, T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat. Rev. Immunol. 2021, 21, 426–440. [Google Scholar] [CrossRef]
- Aminoshariae, A.; Ms, D.D.S.; Kulild, J.C.; Ms, D.D.S.; Fouad, A.F.; Ms, D.D.S. The Impact of Endodontic Infections on the Pathogenesis of Cardiovascular Disease ( s ): A Systematic Review with Meta-analysis Using GRADE. J. Endod. 2018, 44, 1361–1366e3. [Google Scholar] [CrossRef] [PubMed]
- Cintra, L.T.A.; Estrela, C.; Azuma, M.M. ; Queiroz, índia O. de A.; Kawai, T.; Gomes-Filho, J.E. Endodontic medicine: Interrelationships among apical periodontitis, systemic disorders, and tissue responses of dental materials. Braz. Oral Res. 2018, 32, 66–81. [Google Scholar] [CrossRef]
- Cintra, L.T.A.; Gomes, M.S.; da Silva, C.C.; Faria, F.D.; Benetti, F.; Cosme-Silva, L.; Samuel, R.O.; Pinheiro, T.N.; Estrela, C.; González, A.C.; et al. Evolution of endodontic medicine: a critical narrative review of the interrelationship between endodontics and systemic pathological conditions. Odontology 2021, 109, 741–769. [Google Scholar] [CrossRef]
- Segura-Egea, J.J.; Cabanillas-Balsera, D.; Jiménez-Sánchez, M.C.; Martín-González, J. Endodontics and diabetes: association versus causation. Int. Endod. J. 2019, 52, 790–802. [Google Scholar] [CrossRef]
- Cabanillas-Balsera, D.; Segura-Egea, J.J.; Bermudo-Fuenmayor, M.; Martín-González, J.; Jiménez-Sánchez, M.C.; Areal-Quecuty, V.; Sánchez-Domínguez, B.; Montero-Miralles, P.; Velasco-Ortega, E. Smoking and Radiolucent Periapical Lesions in Root Filled Teeth: Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 3506. [Google Scholar] [CrossRef]
- Jiménez-Sánchez, M.; Cabanillas-Balsera, D.; Areal-Quecuty, V.; Velasco-Ortega, E.; Martín-González, J.; Segura-Egea, J. Cardiovascular diseases and apical periodontitis: association not always implies causality. Med. Oral Patol. Oral y Cir. Bucal 2020, 0–0. [Google Scholar] [CrossRef]
- Jakovljevic, A.; Ideo, F.; Jacimovic, J.; Aminoshariae, A.; Nagendrababu, V.; Azarpazhooh, A.; Cotti, E. The Link Between Apical Periodontitis and Gastrointestinal Diseases-A Systematic Review. J. Endod. 2023, 49, 1421–1431. [Google Scholar] [CrossRef]
| Reasons | Excluded studies |
|---|---|
| Not providing the necessary data | Friedlander et al. 2010 [25] Cotti et al. 2011 [12] Glodny et al. 2013 [26] Liljestrand et al. 2016 [27] Chauhan et al. 2019 [11] |
| Some patients in the experimental group did not have atherosclerosis | Frisk et al. 2003 [30] Willershausen et al. 2009 [28] Pasqualini et al. 2012 [29] |
| Not establishing the radiological diagnosis of CAP | Jansson et al. 2001 [31] Cowan et al. 2020 [32] Liu et al. 2023 [33] |
| Author, year | Study design | Subjects | Diagnostic methods for CAP and atherosclerotic condition | Main results |
|---|---|---|---|---|
| Petersen et al. 2014 [34] |
Cross-sectional | Control – 255 Atherosclerotic – 276 |
CT scan Healing scanning from CTs of abdominal aorta |
CAP correlate positively with the aortic atherosclerotic burden. |
| Costa et al. 2014 [35] |
Cross-sectional | Control – 36 Atherosclerotic – 67 |
Periapical radiographs Coronary angiography |
CAP was independently associated with coronary artery disease |
| Gomes et al. 2016 [13] |
Retrospective | Control – 216 Atherosclerotic – 62 |
Ortopantomography Incident CVE |
The number of teeth with CAP in midlife was an independent predictor of CVE |
| González-Navarro et al. 2020 [36] |
Cross-sectional | Control – 48 Atherosclerotic – 83 |
Ortopantomography Having suffered an atherotrombotic CVE |
CAP was significantly associated with atherotrombotic CVE |
| Malvicini et al. 2024 [37] |
Cross-sectional | Control – 38 Atherosclerotic – 27 |
Ortopantomography Carotid wall thickness Doppler ultrasound |
CAP was associated with 5-fold increased odds of having carotid plaques |
| Authors and year | No. subjects | Atherosclerotic patients |
Control subjects | Odds Ratio (95%CI) | p | ||
| CAP / Total | CAP Prevalence (%) |
CAP / Total | CAP Prevalence (%) |
||||
| Petersen et al. 2014 [34] | 531 | 228/276 | 82.6 | 161/255 | 63.1 | 2.77 (1.86-4.15) |
< 0.001 |
| Costa et al. 2014 [35] | 103 | 34/67 | 50.7 | 9/36 | 25.0 | 3.09 (1.26-7.55) |
0.012 |
| Gomes et al. 2016 [13] | 278 | 18/62 | 29.0 | 43/216 | 19.9 | 1.65 (0.87-3.13) |
0.126 |
| González-Navarro et al. 2020 [36] | 131 | 39/83 | 47.0 | 12/48 | 25.0 | 2.66 (1.22-5.82) |
0.013 |
| Malvicini et al. 2024 [37] | 65 | 18/27 | 66.7 | 5/38 | 13.2 | 13.20 (3.84-45.38) |
< 0.001 |
| OVERALL | 1,108 | 337/515 | 65.4 | 230/593 | 38.8 | ||
| Sample selection | Outcome | Risk of bias | ||||||
| Representativeness of the sample (max 3) |
Sample size calculation (max 1) | Atherosclerotic condition (max 2) |
Outcome assessment (max 2) | Type of radiograph (max 2) |
Inclusion of third molar (max 1) | No. of observers (max 1) |
||
| Petersen et al. 2013 [34] | ** | ** | * | 5 (moderate) | ||||
| Costa et al. 2014 [35] | * | * | ** | ** | * | 7 (moderate) | ||
| Gomes et al. 2016 [13] | * | ** | * | * | 5 (moderate) | |||
| González-Navarro et al. 2020 [36] | * | * | * | ** | * | 6 (moderate) | ||
| Malvacini et al. 2024 [37] | * | ** | * | ** | * | 7 (moderate) | ||
| OVERALL | 3 | 1 | 8 | 2 | 7 | 4 | 5 | 30 (moderate) |
| Certainty assessment | Certainty | Importance | ||||||
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations |
||
| Atherosclerosis – apical periodontitis | ||||||||
| 5 | Observational studies | Not seriousa |
Not seriousb |
Not serious |
Seriousc | OR: 2.94 (1.83-4.74) p<0.01 |
 Low |
IMPORTANT |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





