1. Introduction
Literature on abdominis recti diastasis is still limited. In 2021, the European Hernia Society (EHS) established a classification method based on the width of the rectus abdominis, considering muscle separation, post-pregnancy status, and the presence of a concomitant hernia. Impaired body image is the most common and relevant symptom. Most published literature correlates the widening of the
linea alba to parity, and this effect has been found in prospective studies, with a positive correlation between parity and RD up to 12 months postpartum [
1,
2,
3].
In the late 1980s, the mini abdominoplasty was described to address RD and flaccidity, aiming to correct deformities of the lower abdominal wall. Recently, advancements in minimally invasive techniques for abdominal wall reconstruction have made it possible to also address cranial deformities of the abdominal wall through the Subcutaneous Onlay Laparoscopic Approach (SCOLA) technique and Minimally Invasive Lipoabdominoplasty Approach (MILA), which add liposuction and skin retraction devices to the plication of the RD [
4,
5,
6,
14,
15]. Considering these advancements, we raised concerns about whether they are sufficient to address the skin flaccidity resulting from parity.
We aimed to demonstrate an endoscopic surgical correction of RD with a novel approach for mini-abdominoplasty minimally invasive (MAMI) abdominal contouring.
2. IDEAS
A widening greater than 2 centimeters of the
linea alba is typically considered for surgical correction according to the European Hernia Society (EHS) [
2]. The latest trends MILA and SCOLA approach for RD are indicated for patients with a body mass index (BMI) up to 28, considering only height and weight. Nevertheless, some may find this insufficient for certain types of patients. Despite advancements in skin retraction, there is still no evidence of how the devices may affect postoperative outcomes when added to these procedures. [
5,
8,
10,
14,
15].
The growing attention to minimally invasive procedures raises questions about patients being submitted to RD correction, even though these procedures are limited to thin patients with small abdominal hernias without skin flaccidity [
7,
8].
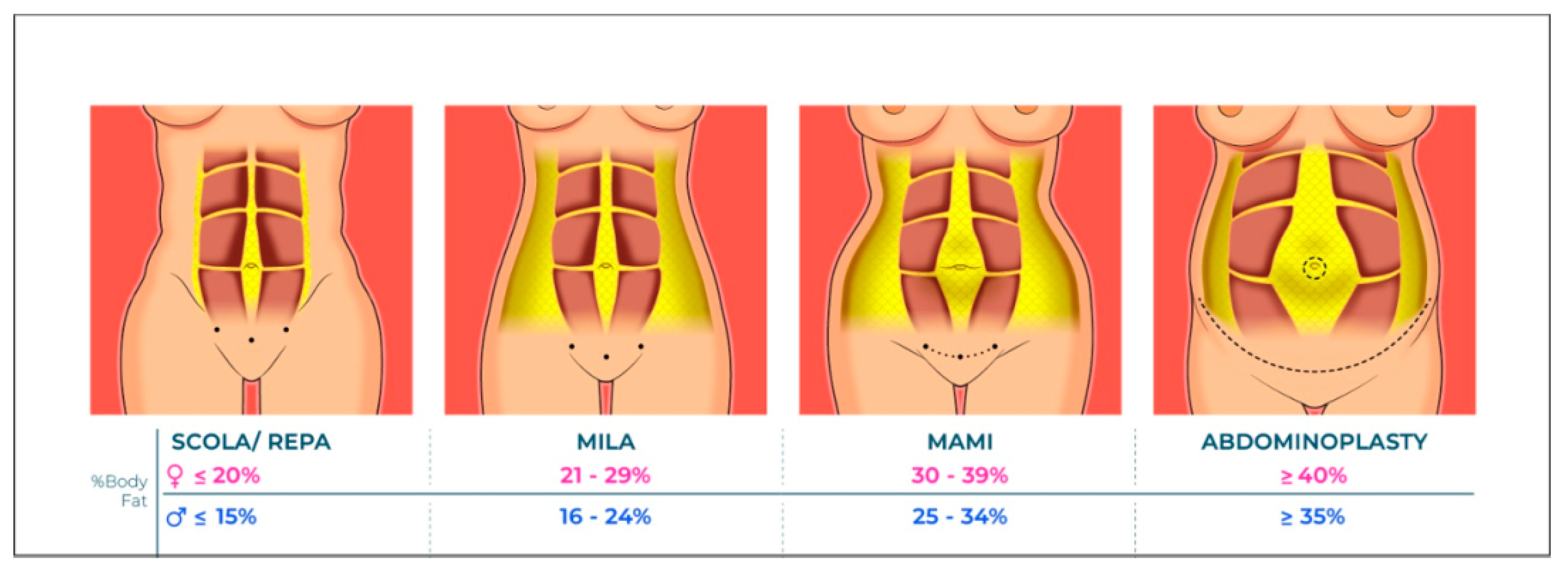
To better assess the ideal treatment for individualized patients, other measures besides BMI should be considered. BMI alone cannot predict skin flaccidity or the patient's body composition. For non-obese patients, bioimpedance, with or without the skin pinch clinical test and fat mass index, could provide more information on how to proceed with surgical treatment [
12].
On the other hand, thin patients with skin flaccidity and a clinical or imaging diagnosis of RD that could be indicated for Mini Abdominoplasty with Minimally Invasive Approach (MAMI) could benefit from a minimally invasive surgery.
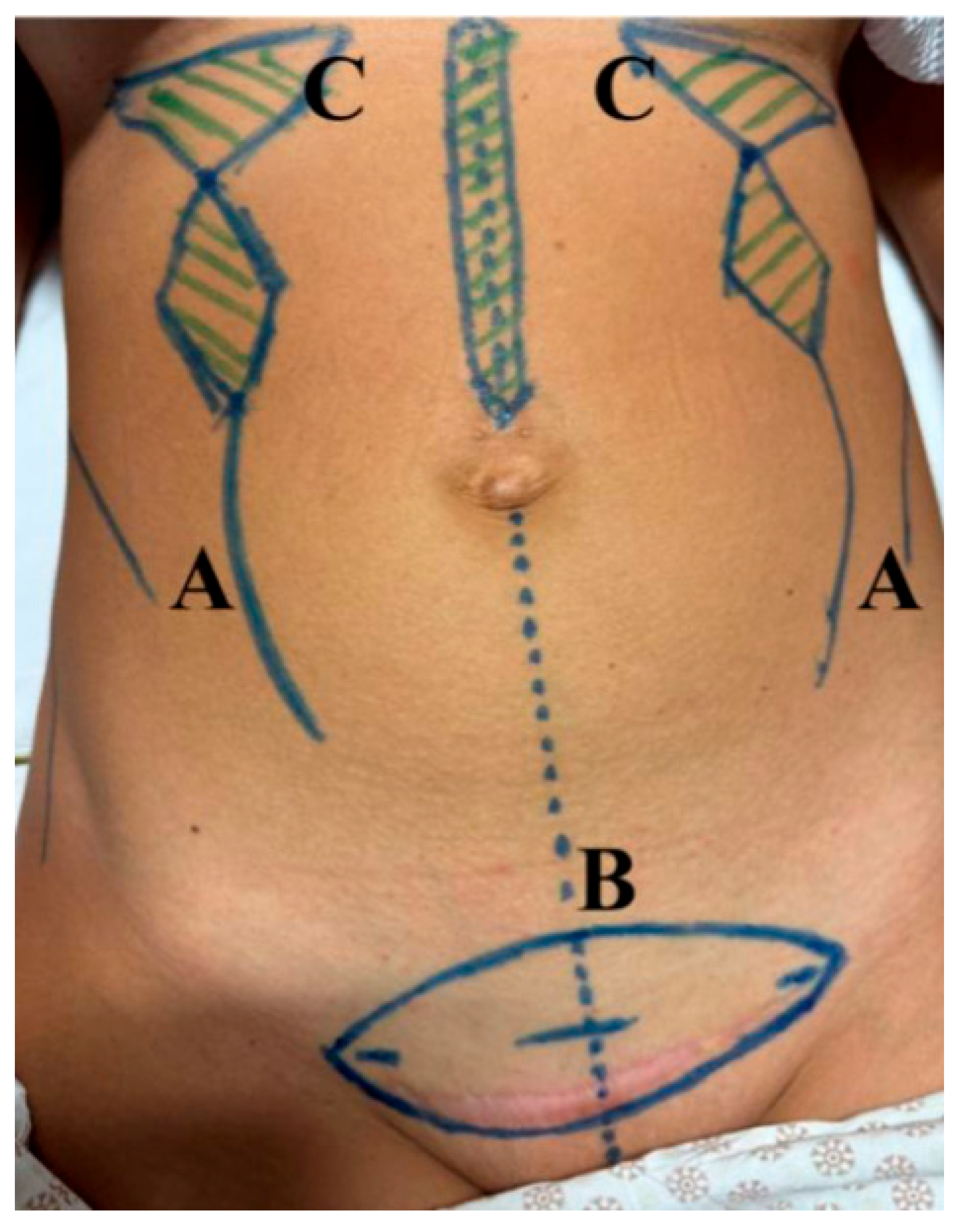
Steps we follow on MAMI approach: 1-Liposuction; 2 - Supraponeurotic repair of midline hernias and diastasis; 3- Skin retraction technology; 4- Cesarean scar resection or skin resection (or small suprapubic incision in case of natural birth or nulligravida women).
3. Results
The main purpose of this study is to address a possible misfit indication for endoscopic surgical correction of RD, based on the common presentation of this condition. Although RD is not related to morbidity as there is no true defect in the abdominal wall thus it cannot lead to incarceration, it is a common complaint in the postpartum period. Up to a third of these patients can develop a widening of the
linea alba [
2,
7].
Several techniques had been described following the involvement of general surgery in the field, making significant contributions since a minimally invasive approach can be used for RD assessment [
8,
10,
14,
15]. Liposuction can enhance the treatment, aiming for better aesthetic correction in patients with RD without skin laxity. Even if MILA can be performed with liposuction and skin-retraction energy, patients with moderate percentage of body fat may need more aggressive measures to reach the same aesthetic results [
8,
10,
14,
15]. (
Figure 1)
Furthermore, patients diagnosed with diastasis in usual practice who show no signs of skin laxity could develop it after MILA or SCOLA correction due to lack of skin compliance after RD correction on the median line. This effect might be due to skin bulging after the suture of the rectus sheath, causing the detached skin to become loose [
7,
14,
15].
Meanwhile, Mini Abdominoplasty is still performed for patients with those conditions. This technique is primarily for patients wanting smaller scars, thus there is still indication for skin excision due to laxity, common after childbirth. Even with advancements in skin retraction technology, there is still a need for clarity on long-term performance of those devices. In this regard, the wedge excision followed by RD assessment remains the most common approach for skin laxity [
4,
5,
9,
10]. (
Figure 2)
For surgeons, the Mini Abdominoplasty approach is not the most ergonomic surgery. The subcutaneous dissection and RD correction performed through a small incision, require an uncomfortable positioning and excessive skin traction, potentially resulting in a painful recovery for both the surgeon and the patient. Furthermore, the lesser time of exposed subcutaneous could indulge in less occurrence of surgical site infection, as it occurs in ventral hernia repair [
13].
Nevertheless, the proposed name for the technique is performed by the surgeon and assistant in a standing position, with the subcutaneous tissue expanded by insufflated CO2, eliminating the need for skin traction with a wider surgical field. Following RD correction, this procedure could allow umbilical scar fixation without the need for a neo-umbilicus. (
Figure 3)
In our experience, Mini Abdominoplasty with a Minimally Invasive Approach (MAMI) has the potential to enhance outcomes, reducing pain and bulging after surgery for patients requiring RD correction with skin laxity.
Therefore, the conventional BMI assessment for MILA correction might not be the best approach for surgery indication based on reviewed literature.
4. Conclusions
MAMI surgery has been shown to be a safe and reproducible approach for selected women who wish to restore the feminine characteristics of the body after childbirth and have a rapid recovery. It may have better aesthetic results than the traditional full abdominoplasty due to the minimized scar and the muscle plication that provides definition of the body contour.
It reduces the risks of mini abdominoplasty in relation to the exposure of subcutaneous tissue for a long time, and improves the quality of visualization for dissection of the subcutaneous tissue and treatment of associated diastasis and hernias.
Author Contributions
Conceptualization, R.F.G, T.M. and A.C.C.; methodology, R.F.G, A.C.C and R.N.; investigation, R.F.G, T.M., A.C.C. and R.N.; data curation, R.F.G.; writing—original draft preparation, R.F.G, A.C.C.; writing—review and editing, R.F.G. and R.N.; visualization, X.X.; supervision, X.X.; project administration, X.X.; funding acquisition, Y.Y. All authors have read and agreed to the published version of the manuscript.
Funding
The authors have no sources of funding to declare for this manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval were waived for this study due to the data used in this technical note are completely de-identified, so there is no risk to individual privacy.
Informed Consent Statement
Patient consent was waived due to the data used in this technical note are completely de-identified, so there is no risk to individual privacy.
Data Availability Statement
Data sharing is not applicable (only appropriate if no new data is generated or the article describes entirely theoretical research).
Conflicts of Interest
The authors have no conflict of interest to declare.
References
- Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016 Sep;50(17):1092-6. [CrossRef] [PubMed] [PubMed Central]
- Hernández-Granados P, Henriksen NA, Berrevoet F, Cuccurullo D, López-Cano M, Nienhuijs S, Ross D, Montgomery A. European Hernia Society guidelines on management of rectus diastasis. Br J Surg. 2021 Oct 23;108(10):1189-1191. [CrossRef] [PubMed] [PubMed Central]
- Turan V, Colluoglu C, Turkyilmaz E, Korucuoglu U. Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekol Pol. 2011 Nov;82(11):817-21. [PubMed]
- Wilkinson, TS. Mini-abdominoplasty. Plast Reconstr Surg. 1988 Nov;82(5):917-8. [CrossRef] [PubMed]
- Greminger, RF. The mini-abdominoplasty. Plast Reconstr Surg. 1987 Mar;79(3):356-65. [CrossRef] [PubMed]
- di Diego, JM. Endoscopic Lipoabdominoplasty. Plast Reconstr Surg Glob Open. 2021 Jan 26;9(1):e3346. [CrossRef] [PubMed] [PubMed Central]
- CLAUS CMP, et al.. SUBCUTANEOUS ONLAY LAPAROSCOPIC APPROACH (SCOLA) FOR VENTRAL HERNIA AND RECTUS ABDOMINIS DIASTASIS REPAIR: TECHNICAL DESCRIPTION AND INITIAL RESULTS. ABCD, arq bras cir dig [Internet]. 2018;31(4):e1399. [CrossRef]
- di Diego, JM. Endoscopic Lipoabdominoplasty. Plast Reconstr Surg Glob Open. 2021 Jan 26;9(1):e3346. [CrossRef] [PubMed] [PubMed Central]
- Malone, C.H., Walters, N., Stroh, R. et al. New Technologies in Skin Tightening. Curr Otorhinolaryngol Rep 9, 422–435 (2021). [CrossRef]
- Bank, David E. MD1,2; Perez, Maritza I. MD1,3. Skin Retraction After Liposuction in Patients Over the Age of 40. Dermatologic Surgery 25(9):p 673-676, September 1999. |. [CrossRef]
- Bozola AR. Abdominoplasty: same classification and a new treatment concept 20 years later. Aesthetic Plast Surg. 2010 Apr;34(2):181-92. [CrossRef] [PubMed]
- Peltz G, Aguirre MT, Sanderson M, Fadden MK. The role of fat mass index in determining obesity. Am J Hum Biol. 2010 Sep-Oct;22(5):639-47. [CrossRef] [PubMed] [PubMed Central]
- Zhang Y, Zhou H, Chai Y, Cao C, Jin K, Hu Z. Laparoscopic versus open incisional and ventral hernia repair: a systematic review and meta-analysis. World J Surg. 2014 Sep;38(9):2233-40. [CrossRef] [PubMed]
- Claus CMP, DI-Biasio GA, Ribeiro RD, Correa MAMF, Pagnoncelli B, Palmisano E. Minimally invasive lipoabdominoplasty (MILA) tactic. Rev Col Bras Cir. 2024 Jun 14;51:e20243692. English, Portuguese. [CrossRef] [PubMed]
- Malcher F, Lima DL, Lima RNCL, Cavazzola LT, Claus C, Dong CT, Sreeramoju P. Endoscopic onlay repair for ventral hernia and rectus abdominis diastasis repair: Why so many different names for the same procedure? A qualitative systematic review. Surg Endosc. 2021 Oct;35(10):5414-5421. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).